Powerpoint - West Texas AHEC
advertisement
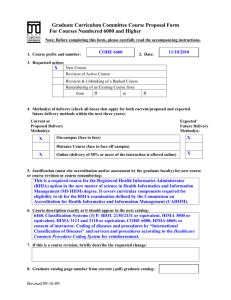
Crossroads Conference ICD-10 Industry Update Susan H. Fenton, PhD, RHIA Asst. Dean for Academic Affairs UT School of Biomedical Informatics @ Houston Agenda Policy • The delay • ICD-11 • SNOMED Practical impacts • Clinical documentation • Coding productivity • Quality Measures The Delay • H.R. 4302 • SEC. 212. DELAY IN TRANSITION FROM ICD–9 TO ICD–10 CODE SETS. The Secretary of Health and Human Services may not, prior to October 1, 2015, adopt ICD–10 code sets as the standard for code sets under section 1173(c) of the Social Security Act (42 U.S.C. 1320d–2(c)) and section 162.1002 of title 45, Code of Federal Regulations. • $1 billion to $6.6 billion additional – CMS Latest Update “On April 1, 2014, the Protecting Access to Medicare Act of 2014 (PAMA) (Pub. L. No. 113-93) was enacted, which said that the Secretary may not adopt ICD-10 prior to October 1, 2015. Accordingly, the U.S. Department of Health and Human Services expects to release an interim final rule in the near future that will include a new compliance date that would require the use of ICD10 beginning October 1, 2015. The rule will also require HIPAA covered entities to continue to use ICD-9-CM through September 30, 2015.” Provider Responses Part B News, 73% of providers plan to stick with their original ICD- 10 implementation plans, despite the delay, EHR Intelligence reports (Bresnick, EHR Intelligence, 4/24). How providers feel about the delay. Specifically: • 34% of organizations ready but appreciate additional time; • 31% of organizations disappointed with the delay; • 20%+ of organizations frustrated because physicians now might want to delay training; and • 13.5% of organizations happy with the delay because they would not have been ready otherwise (Marbury, Medical Economics, 4/23). CMS ICD-10 Claims Submission Testing Conducted in March 2014 • 2,600 participating organizations; 50% were clearinghouses • 127,000 claims submitted with ICD-10-CM/PCS codes • 89% of claims were accepted • Some claims included intentional errors to ensure the system would reject appropriately Contact local MAC for acknowledgment testing details More end-to-end testing in 2015 ICD-11 Release delayed to 2017 – WHO Derived from SNOMED Compatible with EHRs Participate @ http://www.who.int/classifications/icd/revision/icd1 1faq/en/ SNOMED Focused on clinical information Compatible with EHRs 311,000 active concepts 33% agreement on core concept choice • Andrews, J.E., Richesson, R.L., and Krischer, J. (2007) SNOMED CT Coding of Clinical Research Concepts, Journal of AMIA, 14(4), 497-506. So, why move at all? • Public health • Quality patient care • Research • Reimbursement Clinical Documentation Improvement • Laterality: No longer accept injuries to limbs or bilateral organ conditions without laterality. • Paralytic syndromes require right/left and dominant/nondominant • Infectious organisms. How can we help clinicians include these in their documented diagnoses? Injuries • A for Initial Encounter – active initial treatment in ER, surgery or new clinician • D for Subsequent – healing or recovery such as cast change or aftercare • S for Sequela – complications or conditions as a direct result of the injury. Examples include scars or frozen joint Fractures • Open, including Type vs. Closed • Routine vs. Delayed healing • Nonunion vs. Malunion • Displaced vs. Nondisplaced • Many types, transverse, comminuted, or spiral to name just a few Clinician-specific Efforts Track use of unspecified codes by clinician •Appropriate or not? Random coding of records in ICD-10-CM/PCS to determine adequacy of documentation •Feedback •Evaluation criteria Inpatient Coding Productivity • 54 records • 6 coders • ICD-9-CM Avg Coding Time – 25.51 • ICD-10-CM/PCS Avg Coding Time – 43.23 • Overall on average it took 17.72 minutes or 69% longer to code a record in ICD-10CM/PCS Coding Quality or Inter-rater Reliability • ICD-9-CM Diagnostic = .68 • ICD-9-CM Procedural = .61 • ICD-10-CM = .49 • ICD-10-PCS = .42 Quality vs. Minutes/Record • Spearman’s Correlation •Correlation Coefficient = -.424 •P-value = .027 • As the time spent per record increases, the coding quality decreases Veterans Health Administration Inpatient Coding Productivity • 382 inpatient records • 65% decrease in productivity • 12.5 minute decrease without procedures • 20 minute decrease with procedures • Non-OR procedures accounted for longest Veterans Health Administration Ambulatory Coding Productivity • 1,024 ambulatory care records • 6.7% decrease in productivity • Longest time to code ER and Therapy • Productivity recovered within 2 months Comparability Factors or Ratios • Comparability, aka bridge-coding, for longitudinal data comparison • Performed for ICD-9 to ICD-10 for Cause of Death • http://www.cdc.gov/nchs/data/nvsr/nvsr49/nvsr49_02. pdf • Must dual code same set of records • 𝐶𝑖 = 𝐷𝑖 ICD10 𝐷𝑖 (ICD9) Calculating the Comparability Factors • Frequencies run for ICD-9-CM and ICD-10-CM diagnostic codes • Used the 2013 General Equivalence Maps • Used the July 2, 2013 National Hospital Inpatient Quality Measures, Appendix A (ICD-9) and Appendix P (ICD-10) Joint Commission Core Measure Comparison (ongoing analysis) Missing ICD-9-CM Cases for AMI I21.02 – STEMI I21.4 – Acute involving diagonal subendocardial coronary artery MI 410.72 – Subendocardial infarction 410.12 – AMI of other anterior wall 6 1 Extra ICD-9 Cases for Respiratory Failure J96.01 – Acute hypoxemic respiratory failure 518.81 – Acute Respiratory Failure 27 J96.02 – Acute hypercapnic respiratory failure 4 In the Final Analysis • Implementation now slated for 10/1/2015 • Review insurance and vendor contracts • More time for system upgrades • Continue documentation improvement • Maybe consider Computer-assisted Coding • Identify potential longitudinal data concerns Questions Thank you to Texas Tech and the West Texas AHEC. Contact Information • Susan H. Fenton, PhD, RHIA, FAHIMA • Assistant Dean, UT SBMI • susan.h.fenton@uth.tmc.edu