Lower Extremity Wounds
advertisement
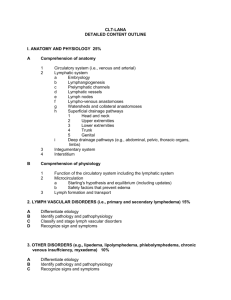
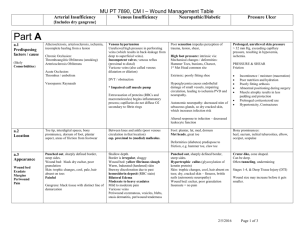
Lower Extremity Wounds Objectives • Differentiate between arterial, venous, and diabetic wounds • Illustrate wound treatment techniques for lymphedema, venous, arterial, and diabetic wounds Epidemiology Sen et al; 2009 • 17.9 million people in the US have been diagnosed with diabetes – 25% of this population will develop ulcers – 12% of those ulcers result in amputation • 1.69% of the US population has venous wounds Arterial Wounds Examination • History of arterial disease • Blood flow to the extremity – Pedal pulses (many times unable to locate) – Ankle Brachial Index (ABI) • Note edema • Skin changes: decreased hair, shiny skin, dark color, decreased temperature, decreased muscle bulk • Gangrene of toes • Nail changes Arterial Wound Characteristics • Usually associated with cardiovascular/arterial disease • Appearance: Deep wounds, “punched out”, irregular boarders, may have darker coloring of tissue, dry, may have edema • Location: Anywhere the artery is occluded, more likely to be distal (foot) and lateral leg • Pain: Elevation of the legs, walking, sometimes at rest; relieved by dependent positioning Basic Treatment • • • • • • • • Keeping the wound clean and dry Preventing infection and trauma Keep the leg(s) in a dependent position Create moisture with dressings Passive exercises Increase temperature Avoid constricting socks, clothing Good nutrition Other Treatments • Wounds are very slow to heal • Medications to increase blood flow • Surgical: – Revascularization – Amputation Diabetic Wounds Examination • Medical history of diabetes • Check sensation – Monofilament test for protective sensation • Check blood flow to the area – Pedal pulses (may not be present) – Ankle Bracial Index (ABI) • Note surrounding skin (callous formation) • Note foot deformaties Diabetic Wounds • Diabetes effects multiple body systems. May see a mixed wound • Associated with diabetic neuropathy – where nerves are affected • Foot deformities are common • Usually caused by several factors: – – – – Decreased sensation Arterial insufficiency Unable to monitor feet Competition for time and resources with other associated illnesses – Denial – Mis-information Common Foot Deformities Seen With Neuropathy • Charcot Foot Diabetic Wound Characteristics • Appearance: Round or elliptical, may see a callous on surrounding tissue • Location: Areas of pressure or shearing forces, primarily below the ankle • Pain: May not have any primarily due to decreased sensation Basic Treatment • Off loading (removing the pressure to the wound area) – Using assistive devices to walk – Transfer to wheelchair only Important to monitor weight bearing Balance deficits may increase • Use specialized foot wear at all times • Monitor skin of other areas of the foot Easily become infected Types of Off Loading • Shoes • Splints Skin Care Guidelines • • • • Keep feet dry Pay close attention to between the toes Diabetic socks Management of fungal infections of toes and toenails • Use pH balanced lotions to keep leg and periwound skin healthy • Avoid soaking Other treatments • • • • • • • • Improved control of diabetes Debridement – removal of dead tissue Dressings Casting Management of infection Hyperbaric oxygen (HBO) Increasing vascularization /medical management Amputation Signs and Symptoms of Infection • • • • Very similar to inflammation Increased temperature Increased pain Purulent drainage (contains pus) LOOK FOR CHANGES Venous Wounds Examination • • • • Pulses should be present Look for edema, varicose veins Note type and amount drainage Signs and symptoms of infection Venous Wound Characteristics • Appearance: Leg may have edema, vericose veins, and hemosideran staining. – Wound looks “healthy”(beefy, red), may have excessive moisture, shiny, irregular boarders of wound – Surrounding skin may be macerated, crusting, scaling (dry appearance) • Location: “Gaiter” area of the lower leg, primarily near the medial malleolus • Pain: Sometime, dull, aching. Should be relieved by elevation/rest. Many patients with venous hypertension/varicose veins will also have arterial problems. Wounds may be mixed. Basic Treatment • Dressings that focus on controlling drainage May need frequent dressing changes • • • • Protecting periwound Leg elevation Compression Walking with compression Lymphedema Lymphedema Defined • Accumulation of lymphatic fluid in the interstitial tissue • Different from venous insufficiency because there is damage to the lymphatic system • Untreated venous insufficiency can lead to lymphedema • Causes: Primary – present at birth or onset at puberty, adulthood (unknown cause) • Secondary (most common) – surgery especially when lymph nodes removed, radiation, trauma, infection Lymphedema Characteristics • Appearance: – Swelling usually begins distally and will appear worse distally. – One limb will be larger than the other. – Dorsal hump – Pitting edema in earlier stages. Left untreated, skin will become hard, fibrous with brown staining • Location: Extremities but at times in the face and trunk • Pain: Not usually present but high risk for infection (cellulitis). Normally will start by the extremity feeling heavy. Venous Insufficiency Lymphedema Treatment • Best treated by Certified Lymphedema Therapists • Complete decongestive therapy – – – – Compression Manual lymph drainage (MLD) Exercises Skin/nail care Patients with lymphedema must always wear compression garments Compression Common Types: • Compression garmets (stockings) • Lymphedema wraps (short stretch bandages) • Ace bandages (long stretch bandages) • Compression pumps • Unna’s boots • Other compression systems Contraindications for Compression Therapy Absolute Contraindications • Ruling out arterial insufficiency is important • ABI <0.8 • Suspected/untreated DVT • Phlebitis Relative Contraindications • CHF • Pulmonary edema • Kidney failure • Decreased sensation