EPBI 467 Cost-Effectiveness Analysis in Health Care
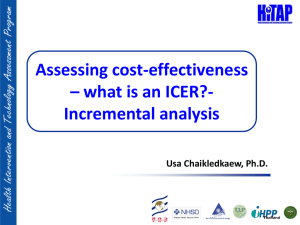
advertisement
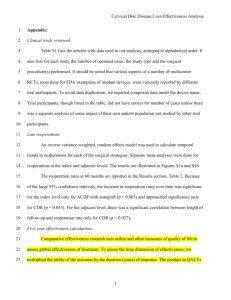
Mendel E. Singer, PhD MPH Associate Professor Dept. of Epidemiology and Biostatistics mendel@case.edu Cost is not the same as charges Cost is more than just a transfer of money Medical Costs Office visit, lab test, hospitalization Non-Medical Costs Lost time, Lost wages, lost productivity, transportation Perspective What costs you include depends on the perspective of the analysis. Patient, Payer, Societal (all costs regardless of who pays) What is the cost of a Prescription? Cost to Patient? Cost to Insurer? Societal Cost • Micro-costing: Detail every input ▪ ▪ ▪ ▪ Time-motion studies Every person involved, how long Equipment used (aging) Overhead • Gross Costing ▪ Reimbursement Rates as Proxy • • • • Medicare Medicaid 3rd Party Insurer Specific Institution’s Estimate Inflation Used to adjust old cost estimates to a more recent year All cost estimates must be from the same year Bureau of Labor Statistics Medical Consumer Price Index ▪ Medical Services ▪ Medical Equipment Discounting Would you rather have $100 now or in 20 years? After adjusting for inflation? Opportunity Cost – what you could have done with the money This is necessary to compare costs now to those incurred downstream. Note: discounting is net of inflation – i.e. after adjusting for inflation Structured methodology for decision making Map out the different possibilities Compares 2 or more treatment strategies Multi-step strategies that model actual practice Could also use purely for modeling natural history ▪ Really a simulated longitudinal Trial ▪ Treatment for Hepatitis C, get estimates of % progressing to ▪ Cirrhosis, Advanced liver disease, Transplant, Liver cancer E.g. what would happen if …. Single measure for comparison Can do a series of measures Define the study population Identify treatment alternatives Select outcome measure Model course of disease Populate model with data Mostly from literature Cost sources ▪ Medicare reimbursement rate, Cost of drugs ▪ Claims data analysis Analyze Sensitivity analysis Uncertainty in the data estimates Reference Case 60-year old male 4 cm abdominal aortic aneurysm Otherwise, patient is in good health Surgery vs Watchful Waiting Time horizon: 1 year Outcome Measure: Survival Alive = 1 Dead = 0 Abdominal Aortic Aneurysm Reference Case: 60-year old male, 4 cm aneurysm, good health Strategies: Surgery vs Watchful Waiting Outcome Measure: Survival at 1 year (alive = 1, dead = 0) 1. At each node there is a number in a box indicating the mean (average) outcome. 2. At all terminal nodes, it first shows the outcome score associated with that result, and then shows the probability of the path ending in that terminal node. Name: Interests: Specialty: Darth Vader, M.D. Cost-effective health care End of Life Care Based on the decision analytic model Now track both cost and effectiveness Cost vs. Effectiveness What’s a good deal for the money? Really a simulated longitudinal Trial Treatment for Hepatitis C ▪ Get estimates of % progressing to: ▪ Cirrhosis, Advanced liver disease Outcomes Research/Quality Assurance Practice Guidelines Health Policy Pharmaceuticals - Justifying new drugs Providers and Insurers Identify research priorities Demonstrate need for large trials Complexity of decisions Many potential complications Information overload Structures the decision process Published studies too narrowly focused Customizable Simulate strategies unable to test in practice Poor Data Lack of data “Wrong” data Incomplete data Funding Poor federal funding Short-term focus of HMOs, insurers Wrong comparator Missing strategies Too complex Wrong population Timeliness Strings attached (private funding) Cost-Minimization Cost only (assumes equal effectiveness) Cost-Benefit Analysis Values cost and health in monetary units Cost-Effectiveness Analysis Objective measure of effectiveness Cost-Utility Analysis Subjective measure of effectiveness Often the measure is Quality-Adjusted Life Years (QALYs) ▪ Years of life are weighted by a utility score that measures patient preferences for a particular state of health. Huh? Utility – What does the term really mean? Valuation under uncertainty Measure of Patient Preference Scale 0 – 1, where: 1 = Full Health 0 = Death Possible to have negative utility (< death) True Scale – same meaning across scale 1.000 0.998 0.75 0.62 0.00 Full Health Well, Aspirin therapy Mild Stroke with residua Moderate COPD Death 2 years of life with moderate COPD: 2 x 0.62 = 1.24 QALYs Never Use Average Cost-effectiveness Ratios Which do you prefer? ▪ 1 brand new Rolls Royce for $25 ($25 each) ▪ 2 brand new Rolls Royces for $100 ($50 each) Always use incremental C-E Ratios (Difference in Cost) / (Difference in Effectiveness) Possible outcomes One strategy is dominated (cost , effectiveness ), or Is the extra effectiveness worth the extra cost? Cost Effectiveness Drug A $ 100 10.00 QALYs Surgery $1,100 10.05 QALYs Incremental Cost-Effectiveness Analysis Cost Effective. ICER Drug A ------- ------------ --------- Surgery $1,000 0.05 QALYs $20,000/QALY Is this intervention cost-effective? Cost Effectiveness Drug A $ 100 10.00 QALYs Surgery $1,100 10.05 QALYs Incremental Cost-Effectiveness Analysis Cost Effective. ICER Drug A ------- ------------ --------- Surgery $1,000 0.05 QALYs $20,000/QALY Is this intervention cost-effective? Common threshold: $50,000 - $100,000/QALY International studies often use 1 GDP/QALY, though WHO suggests: <1 GDP is very cost-effective From 1-3 GDP is cost-effective Decision analytic modeling is an objective method for combining all the complex information of long-term management of disease to compare different treatment strategies on both effectiveness and cost. The models also produce estimates of important long-term clinical outcomes and utilization. Comparative and Cost-Effectiveness Research 2 days of Comparative Effectiveness Research within the context of health Reform, covered from all angles: methods, health policy, impact on payers and providers and patients, ethical/legal/social issues. 3 days crash course in cost-effectiveness analysis CME credits Take as an official course OR pay workshop fee Tentative dates: May 13-14, 15-17. CTSC will send info. Or e-mail: mendel@case.edu Mendel Singer, PhD MPH ….. mendel@case.edu