CCS Guideline on Antiplatelet Therapy for patients with Stable
advertisement
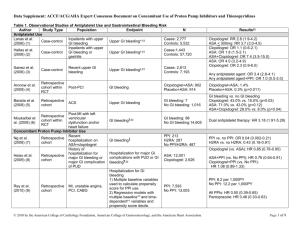
Canadian Cardiovascular Society Antiplatelet Guidelines Antiplatelet Therapy for Secondary Prevention Beyond One Year Following ACS or PCI Working Group: Anil Gupta MD, FRCPC, Pierre Theroux MD, FRCPC Leadership. Knowledge. Community. Objectives Interpret the Canadian Cardiovascular Society Guideline recommendations regarding the use of antiplatelet therapy for patients with stable coronary artery disease. Distinguish when it is appropriate to continue or discontinue dual antiplatelet therapy 1 year post event. Evaluate the evidence supporting the use of antiplatelet agents in patients with stable coronary artery disease. © 2011 - TIGC Mary Mary is a 72 year-old retired teacher who suffered a NSTEMI three years ago. She was managed medically and made an uneventful recovery. Since her event she remains asymptomatic and has no significant comorbidity. © 2011 - TIGC Mary Which of the following are appropriate antiplatelet regimens for Mary? A. ASA 81 mg OD B. Clopidogrel 75 mg daily C. ASA 81 mg + Clopidogrel 75 mg daily D. Any of the above © 2011 - TIGC Benefit of antiplatelet therapy Antithrombotic trialists collaboration ARR 3.5 % 13.5% vs 17.0% NNT 29 © 2011 - TIGC Antithrombotic Trialists, BMJ 2002; 324: 71-86. Absolute benefit of ASA in secondary prevention Baigent C, Blackwell L, Collins R, et al. Lancet 2009;373:1849-60. © 2011 - TIGC Stable CAD ASA VS CLOPIDOGREL © 2011 - TIGC CAPRIE Study design Multicentre, prospective, blinded Study population 19,185 patients with atherosclerotic vascular disease Qualifying conditions Ischemic stroke (>1 week and <6 months) Myocardial infarction (MI) (<35 days) Peripheral Vascular disease Study drugs Clopidogrel 75 mg once daily Aspirin 325 mg once daily Primary endpoint MI, ischemic stroke, or vascular death Treatment duration Up to 3 years (mean 1.6 year) Investigational sites 384 in 16 countries CAPRIE Steering Committee. Lancet 1996;348:1329-1339. © 2011 - TIGC CAPRIE results Relative Risk Reduction* by qualifying entry criteria 7.3 IS (n=6431) -3.7 MI (n=6302) 23.8 PAD (n=6452) 8.7 20 10 ASA better 0 Total (n=1918) 10 20 30 40 Clopidogrel better *Cluster of IS, MI, or vascular death. CAPRIE Steering Committee. Lancet 1996;348:1329-1339. CAPRIE bleeding % of patients with events Aspirin (325 mg/d) Clopidogrel (75 mg/d) Intracranial hemorrhage 0.49 0.35 Gastrointestinal bleeding 2.66 * 1.99 Severe bleeding 1.55 1.38 Any bleeding 9.28 9.27 *p<0.05 CAPRIE Steering Committee. Lancet 1996;348:1329-1339. Stable CAD DUAL ANTIPLATELET THERAPY VS ASA MONOTHERAPY © 2011 - TIGC CHARISMA Study design Clopidogrel 75 mg/day (n=7802) Patients age ≥ 45 years at high risk of atherothrombotic events R (n=15603) Low dose ASA 75162 mg/day Double-blind treatment up to 1040 primary efficacy events* Low dose ASA 75162 mg/day Placebo 1 tablet/day (n=7801) 1-month visit 3-month visit Visits every 6 months * MI (fatal or non-fatal), stroke (fatal or non-fatal), or cardiovascular death; event-driven trial Bhatt DL, Topol EJ, et al. Am Heart J 2004; 148: 263–268. Final visit (Fixed study end date) CHARISMA Inclusion criteria Patients aged ≥45 years with at least one of the following: 1) Documented coronary disease and/or 2) Documented cerebrovascular disease and/or 3) Documented symptomatic PAD and/or 4) Two major or one major and two minor or three minor risk factors Bhatt DL, Topol EJ, et al. Am Heart J 2004; 148: 263–268. Primary efficacy results (MI/troke/CV death) by pre-specified entry category Population RR (95% CI) Prior CV event p value 0.88 (0.77, 0.998) 0.046 (n=12153) Risk Factors Only 1.20 (0.91, 1.59) 0.20 0.93 (0.83, 1.05) 0.22 (n=3284) Overall Population* (n=15603) 0.4 0.6 0.8 Clopidogrel + ASA Better 1.2 1.4 1.6 Placebo + ASA Better * A statistical test for interaction showed marginally significant heterogeneity (p=0.045) in treatment response for the pre-specified subgroups of symptomatic and asymptomatic patients AT=Atherothrombosis Adapted from Bhatt DL, Fox KA, Hacke W, et al. 2006, in press. Stable CAD LONG TERM ANTIPLATELET THERAPY IN PATIENTS WITH PCI © 2011 - TIGC Stent thrombosis Stent thrombosis occurs following 0.5%-2% of stent placements. Major safety concern with rates of mortality as high as 45% Occurs most frequently in the first month after stent implantation (subacute). Cases of late (30 days to 1 year) and very late (> 1 year) stent thrombosis occur particularly in DES recipients. © 2011 - TIGC Stent thrombosis Predictors of late stent thrombosis Drug Eluting Stent Stenting of small vessels Decreased left ventricular function Presence of multiple lesions Advanced age Long segments implanted with overlapping stents Diabetes Stenting of ostial bifurcation lesions ACS Renal failure Suboptimal stent deployment © 2011 - TIGC Stent thrombosis Drug Eluting vs Bare Metal Median time to stent thrombosis 20 p = 0.0003 p = 0.0052 p = 0.04 16 Months 12 8 4 0 DES BMS SES BMS Bavry AA, et al. Am J Med. 2006;119:1056-61. PES BMS Incidence of very late stent thrombosis > 1 Year Per 1,000 pts 7 6 RR = 5.7 p = 0.049 RR = 5.0 p = 0.02 5 p = 0.22 4 3 2 1 0 DES BMS SES BMS Bavry AA, et al. Am J Med. 2006;119:1056-61. PES BMS Discontinuation of Thienopyridine therapy after DES implantation MI patients who stopped thienopyridine therapy by 30 days post-DES were more likely to die during the next 11 months 15 Mortality (%) Continued Discontinued Adjusted hazard ratio 9.0; 95% CI = 1.3 to 60.6 10 P<0.001 5 0 0 1 2 3 4 5 6 7 Months Spertus JA, et al. Circulation. 2006;113:2803–2809. 8 9 10 11 12 BASKET LATE Late thrombotic events following Thienopyridine discontinuation Cardiac death or MI P=0.01 MI P=0.04 6 6 4.9 4.1 4 2 Percentage (%) Percentage (%) 4 1.3 0 2 0 Drug-eluting stents Drug-eluting stents Pfisterer ME, et al. J Am Coll Cardiol. 2006;48(12) 1.3 Bare metal stents Clopidogrel use and long-term outcomes after BMS or DES stenting Adjusted cumulative rates of composite of death or MI using the 6-month landmark analysis Composite of Death or MI 8 Cumulative Incidence (%) DES With Clopidogrel 6 Without Clopidogrel 4 BMS With Clopidogrel 2 Without Clopidogrel 0 6 12 Eisenstein EL, et al. JAMA. 2007;297(2):159-68. 18 Months 24 REAL-LATE/ZEST-LATE Definite Stent Thrombosis Days from Randomization Park SJ, Park DW, et al. N Engl J Med 2010;362 Cumulative Incidence (%) Cumulative Incidence (%) • 2701 patients who had received drug eluting stents • Free of major adverse cardiac or cerebrovascular events and major bleeding for a period of at least 12 months • Randomized open label to receive clopidogrel plus aspirin or aspirin alone Days from Randomization © 2011 - TIGC 24 ® Antiplatelet therapy for secondary prevention beyond 1 year following acute coronary syndrome or percutaneous coronary intervention 1. 2. 3. 4. 5. For all patients with ACS who survive to hospital discharge, indefinite therapy with low-dose ASA (75-162 mg daily) is recommended (Class I, Level A). For patients allergic to or intolerant of ASA, indefinite therapy with clopidogrel 75 mg daily is recommended (Class IIa, Level B). Dual antiplatelet therapy with ASA 75-162 mg daily and clopidogrel 75 mg daily may be considered beyond 1 year in patients with ACS (see post-ACS recommendations) who are medically managed provided the risk of bleeding is low (Class IIb, Level C). For all post-PCI patients, indefinite therapy with ASA 75-162 mg daily is recommended, regardless of type of stent (Class I, Level A). Dual antiplatelet therapy with ASA 75-162 mg daily and clopidogrel 75 mg daily may be considered beyond 1 year in patients with ACS who receive a BMS or DES provided their risk of bleeding is low (Class IIb, Level C). 25 ® Antiplatelet therapy for secondary prevention beyond 1 year following ACS or PCI High-risk Mary What if Mary has additional risk factors for recurrent thrombosis including: Drug eluting stent implantation Diabetes Other prior vascular events including TIA? © 2011 - TIGC CAPRIE Clopidogrel vs ASA in multi-bed disease 15 Annual event rate (%) 10.74% 10 8.35% 5 0 Clopidogrel ASA Events = ischemic stroke, MI or vascular death Lancet 1996; 348(9038):1329-39. CAPRIE Risk reduction in patients with diabetes Annual event rate (%) 25 Clopidogrel 20 21.5% 17.7% 1 5 10 ASA 17.7% 15.6% 11.8% 12.7% 5 0 Non diabetic All diabetic patients With insulin Events = ischemic stroke, MI , vascular death, hospitalization for ischemic events/bleeding Overall benefit p=0.032; multivariate analysis Bhatt DL et al. J Am Coll Cardiol 2000;35 (Suppl A):409 CHARISMA Primary Endpoint (MI/Stroke/CV Death) in patients with previous MI, IS or PAD* N=9,478 “CAPRIE-like Cohort” 8.8% Primary Outcome Event Rate (%) 10 7.3% Placebo + ASA Clopidogrel + ASA 8 6 4 RRR: 17.1 % (95% CI: 4.4%, 28.1%) P=0.01 2 0 0 * Post hoc analysis. 6 12 18 24 30 Months Since Randomization Bhatt DL, Flather MD, Hacke W, et al. J Am Coll Cardiol. 2007;49:1982-1988. High-risk Mary Mary’s additional risk factors suggest more aggressive antiplatelet therapy should be considered. As long as her bleeding risk is low, she may be advised to continue dual antiplatelet therapy with ASA 81 mg + clopidogrel 75 mg. © 2011 - TIGC 31 ® Antiplatelet therapy for secondary prevention beyond 1 year following ACS or PCI Prasugrel or Ticagrelor? No long term secondary prevention studies are available for these agents. Prasugrel should be avoided in patients with: Age > 75 Weight < 60 kg Prior cerebrovascular disease © 2011 - TIGC © 2011 - TIGC