PowerPoint Slides
advertisement
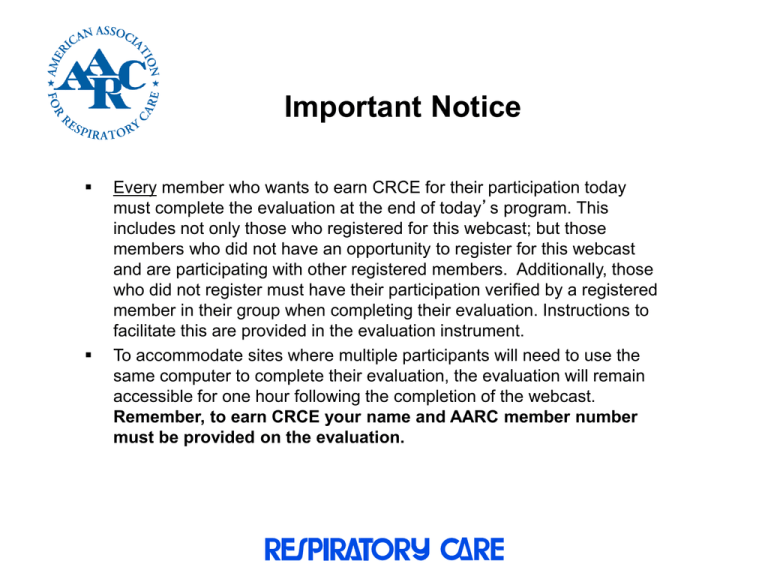
Important Notice Every member who wants to earn CRCE for their participation today must complete the evaluation at the end of today’s program. This includes not only those who registered for this webcast; but those members who did not have an opportunity to register for this webcast and are participating with other registered members. Additionally, those who did not register must have their participation verified by a registered member in their group when completing their evaluation. Instructions to facilitate this are provided in the evaluation instrument. To accommodate sites where multiple participants will need to use the same computer to complete their evaluation, the evaluation will remain accessible for one hour following the completion of the webcast. Remember, to earn CRCE your name and AARC member number must be provided on the evaluation. March 2013 RESPIRATORY CARE Journal Webcast This webcast and any accompanying materials are copyrighted by the American Association for Respiratory Care (AARC). Any public display, sale, copy or distribution of the video or materials may only be undertaken with the prior written consent of the AARC. Copyright 2013 Moderator Shawna Strickland, PhD, RRT-NPS, AE-C, FAARC AARC Associate Executive Director-Education Program Objectives Identify the research question of the study. Identify the study design. Discuss the main results of the study. Discuss the implication of the study on patient care. March 2013 RESPIRATORY CARE Journal Webcast Evaluation of Recruited Lung Volume at Plateau Inspiratory Pressure with Positive End-Expiratory Pressure Using Bedside Digital Chest X-ray in Acute Lung Injury/Acute Respiratory Distress Syndrome Patients Keith D. Lamb, RRT-ACCS Surgical Critical Care Department of Respiratory Care Christiana Care Health System Newark, Delaware USA Chair, AARC Adult Acute Care Section Background • Importance of preventing over distension, and loss of lung volume in ARDS is well known • This requires finding optimal PEEP • Optimal PEEP is difficult to find at the bedside – Ultrasound and Electrical Impedance Tomography – Expensive Equipment • Slow flow Pressure/Volume Curves with New Ventilators • Formal CT which may not be safe for all patients Research Question • Can bedside digital chest radiography be used to evaluate lung recruitment and therefore appropriate PEEP levels to maintain recruitment and avoid over distension? • No COI reported by any of the Authors Methods • Small Prospective Experiment • 14 Patients with ALI/ARDS • Each patient subjected to 5 and 15 of PEEP in a random order for 10 minutes • At the end of 10 minutes a portable/digital CXR was obtained as well as a P/V curve • PaO2, Cst, Cdyn, and change in EELV were measured • Radiological attenuation was measured in 7 predetermined ROI 4 from right and 3 from left Methods • Ratio of lung density (rP15/P5) and the mathematical mean (µP15/P5) were computed • Recruited Volume (Vrec) was determined by P/V curve Inclusion Criteria • ALI/ARDS per consensus conference criteria when using greater than or equal to 5 PEEP. • Greater than or equal to 18 years of age • Intubated and Mechanically Ventilated in the ICU • Continuous IV sedation and analgesia to achieve Ramsay Score of 6 • Vent capable of low inflation flow P/V curve Inclusion Criteria • No pneumothorax per CXR • Pleural Effusion < 500ml estimated via ultrasound • Written informed consent by next of kin Exclusion Criteria • • • • • Thoracic surgery in previous 3 months Recent history of pneumonectomy or lobectomy Pregnancy Patient under guardianship Refusal to participate by next of kin Results • Median value of (rP15/P5) in all 98 lung levels (14 patients/7 levels each) was 0.91. • Values were not significantly different between levels • Median values of Vrec were 288ml • Median value of (µP15/P5) was 0.90 • Significant negative correlation between Vrec and µP15/P5 • Reduction in µP15/P5 correlated with an increase in Cdyn, and an increase in PaO2 between PEEP 15 and PEEP 5 Figure 1 PEEP 5 PEEP 15 Figure 3 Figure 4 Conclusion • Digital CXR done at the bedside in ALI/ARDS patients was able to detect a reduction in density between PEEP of 5 and PEEP 15 which also correlated with Vrec Statistical Analysis • Continuous variables checked by Shapiro-Wilk test • Intra-reader reproducibility was evaluated on all measurements • Primary endpoint was the relationship between µP15/P5 and Vrec • Secondary endpoints were the relationships between µP15/P5 and change in PaO2, Cst, Cdyn, between PEEP 15 and 5 cmH2O. Statistical Analysis • Linear regression analysis was used to evaluate these relationships • A P value < 0.05 was taken as the statistical significance threshold. Discussion • What do these findings mean? There was a significant correlation between a decrease in µP15/P5 (density) on digital CXR and Vrec from Pplat corresponding to PEEP of 5 and to Pplat corresponding to PEEP 15. Recruited volume can be reliably evaluated with fairly intense and pre-planned analysis via bedside digital chest radiography. Discussion • How should these finding impact practice? The impact on practice that this study will have is not clear. This method may have a role when attempting to evaluate lung recruitment and optimal PEEP where slow inspiratory flow P/V curve analysis, EIT, and bedside ultrasound are not available. Discussion • How do these findings related to previous findings from other studies? I could not find similar studies where density ratios were used as surrogates for lung recruitment. P/V curves as well as Lung Ultrasound have been studied. Discussion • What are the study limitations? - Digital CXR not as sensitive to density as other imaging. - Difficult to evaluate for over-distension - Regions of interest may be obscured by lines, tubes, pads etc. - Inter-reader variability would be difficult to control outside of study protocols Discussion • What additional work is needed in this area? Future investigations of this technique to evaluate lung volume would most likely yield similar results. Methods to simultaneously evaluate for over-distension may be helpful in establishing optimal PEEP and recruitment for ARDS patients. Editorial Jean-Jacques Rouby MD PhD & Belaïd Bouhemad MD PhD • The physicians that submitted the accompanying editorial expand on limitations of this study, as well as describe commercially available technology to perform bedside P/V curves as well as inherent limitations of this strategy as well, ie the need for NMB. They also describe bedside ultra-sound techniques and intra-user variability among ultrasononographers. In Summary • Interesting well designed study looking at a potential solution to a real life clinical problem • Small number of patients, but population is similar • Is probably safer than travelling to CT scanner • Is probably cheaper than other methods • May be more difficult to do than it sounds. Need U/S to r/o significant effusion(s) Questions?