PPTX
advertisement

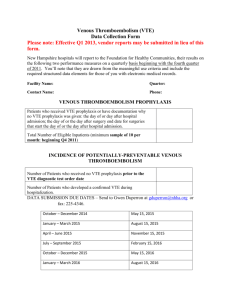
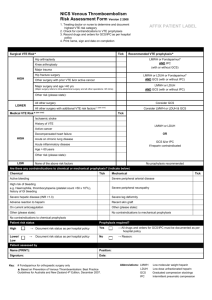
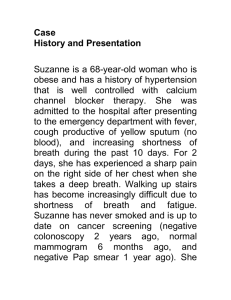
Venous Thromboembolism Reducing the Risk <Name of session> DATE LHD Logo Objectives • Define venous thromboembolism • Heighten awareness – the impact of VTE – the preventable nature of VTE • Discuss importance of – VTE risk assessment – appropriate prescribing of prophylaxis – engaging patients • Demonstrate how to assess VTE risk Venous Thromboembolism • VTE = Deep vein thrombosis (DVT) and/or pulmonary embolism (PE) DVT PE Occurs in deep veins (most commonly in legs and groin) Occurs after DVT dislodges and travels to the lungs Can cause long-term issues – ‘post-thrombotic syndrome’ (PTS) Serious complication which can lead to death PTS affects 23-60% of DVT patients within 2 years Lower-extremity DVT has 3% PE-related mortality rate Patients with PE have 30-60% chance of dying from it What Causes VTE • Virchow’s Triad = categories of factors contributing to blood clot formation Stasis Alteration in normal blood flow VIRCHOW’S TRIAD Endothelial Injury Injury or trauma to the inside of the blood vessel Hypercoagulability Alternation in the constitution of blood causing blood to clot more easily The Impact of VTE • More than 14,000 Australians develop a VTE per year • More than 5,000 of them will die as a direct result • VTE causes 7% of all hospital deaths VTE causes more deaths than bowel Ca and breast Ca VTE Risk Factors VTE Risk Factors Intrinsic Risk Factors Extrinsic Risk Factors Age > 60 years Significantly reduced mobility (relative to normal state) due to injury or illness Obesity (BMI > 30kg/m2) Active malignancy or treatment with chemotherapy Prior history of VTE Use of HRT or oral contraception Pregnancy or post-partum Surgical intervention, particularly major orthopaedic surgery or abdominal/pelvic surgery for cancer Known thrombophilia (including inherited disorders) Active infection Varicose veins Inflammatory bowel disease Hospitalisation • Hospitalisation = ↑ risk of VTE • ~ 50% of VTE cases occur during or soon after hospitalisation – 24% (surgery) – 22% (medical illness) • Incidence 100 times greater in hospitalised patients than community residents Preventing VTE Preventability • Largely preventable • Shift thinking: complication vs adverse event Risk Assessment VTE Prevention Prescribing Appropriate Prophylaxis Assessing Risk • Who should be assessed? ALL adult patients admitted into hospital Others: Preadmission for elective surgery Patient Groups Pregnant and post-partum women Patients discharged from ED with significantly reduced mobility relative to normal state eg in a cast/boot following lower leg injury Assessing Risk • Assess overall VTE risk vs benefit – Assess clotting risk – Assess bleeding risk i.e. contraindications to prophylaxis and/or other bleeding risks • <indicate what tool is available at your facility (State Tool* or Local Tool)> Prescribing Prophylaxis • Patient at risk + nil C/I = prescribe • Two types of prophylaxis: 1. pharmacological 2. mechanical • Ensure C/I to both pharmacological and mechanical prophylaxis have been considered • Evidence-based guidelines NHMRC Guidelines Pharmacological Prophylaxis • Anticoagulants • Alter the process of blood coagulation to prevent VTE formation The coagulation cascade and activity of anticoagulants http://www.healio.com/orthopedics/hip/news/online/%7Ba0ebf835-ae3d-42dfa9e5-ae55b11e0413%7D/new-oral-anticoagulants-for-thromboprophylaxis-aftertotal-hip-or-knee-arthroplasty Pharmacological Prophylaxis • Main anticoagulants include: Drug Class Agents Unfractionated heparin Unfractionated heparin Preferred in patients with renal impairment LMWH Enoxaparin Dalteparin Most commonly used agents Require dosage adjustment in renal impairment Factor Xa inhibitors Apixaban Rivaroxaban Alternative for prophylaxis in post- hip or knee replacement Fondaparinux Alternative for prophylaxis in post- hip or knee replacement and hip fracture surgery Direct thrombin inhibitors Dabigatran Alternative for prophylaxis in prophylaxis posthip or knee replacement Heparinoid Danaparoid Used in heparin-sensitivity or HIT Pharmacological Prophylaxis • Contraindications may include: Contraindications Active bleeding Thrombocytopenia (platelets < 50 x 109/L) End stage liver disease (INR > 1.5) Treatment with therapeutic anticoagulant e.g. warfarin with INR > 2 Severe trauma to head or spinal cord, with haemorrhage in last 4 weeks • Other relative contraindications may exist – weigh risk vs benefit Mechanical Prophylaxis • Devices that increase blood flow velocity in leg veins, reducing venous stasis. • They include: Device Graduated Compression Stockings (GCS) Provide graduated compression, which is firmest at the ankle. Used mainly for ambulant patients Anti-embolic Stocking Standard compression throughout. Used for bedbound or non-ambulant patients Intermittent Pneumatic Compression Device (IPC) Inflatable garment wrapped around legs which is inflated by pneumatic pump. Enhances venous return Foot Impulse Device (FID) Stimulates legs veins to mimic walking and reduce stasis. Used for immobilised patients Mechanical Prophylaxis • Contraindications may include: Contraindications Skin ulceration Lower leg trauma Morbid obesity (where correct fitting of stocking cannot be achieved) Massive leg oedema or pulmonary oedema due to CCF Stroke patients (avoid compression stockings) Other Ways to Help Prevent VTE Empowering Patients • Engage your patients VTE risk factors What they can do to help prevent a VTE Empower with Information Signs and symptoms of VTE What you as their Dr are doing to prevent their development of a VTE Questions For further information: stopclots@cec.health.nsw.gov.au www.cec.health.nsw.gov.au