Funny Thyroid Function Tests
advertisement
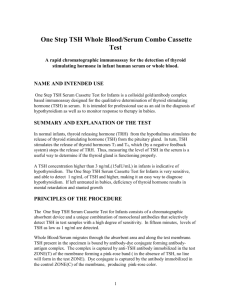
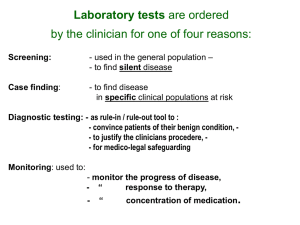
Update in Endocrinology Dr K Foster Consultant Endocrinologist Spire Gatwick Park & East Surrey Hospitals Update in Endocrinology Funny thyroid function tests. Early hyperparathyroidism. Vitamin D Deficiency. Cancer & Diabetes PCOS. Funny thyroid function tests. UK Guidelines for the use of Thyroid Function Tests. (Assn. Clin. Bioch.. Brit. Thy. Assn., 2006). Management of Thyroid Dysfunction during Pregnancy….. (Endo. Soc. 2009). The Diagnosis and Management of Primary Hypothyroidism (RCP & al 2006). Thyrotoxicosis Funny Thyroid Function Tests. TSH = 0.01mu/l, fT4 = 33.2 pmol/l. Thyrotoxic. Subclinical Thyrotoxicosis. TSH = < 0.3mu/l, fT4= 19.0pmol/l. Would you treat?, Repeat?,check T3 or watch? = Hypothyroidism Funny Thyroid Function Tests TSH = > 10mu/l, fT4 = <10pmol/l, Hypothyroid and treat if markedly abnormal or symptomatic Borderline and subclinical hypothyroidism, (TSH = 3.3-7, fT4 = >12). Before lifelong treatment, repeat TFTs in 3/12, treat if symptomatic (or strongly positive anti-thyroid antibodies). Severe myxoedema Funny Thyroid Function Tests TSH = 2.4mu/l, fT4 = 10.2pmol/l. Patient is tired & constipated. Diagnosis? Action? Funny Thyroid Function Tests TSH =2.4mu/l, fT4 = 10.2pmol/l. Probable sick euthyroid syndrome, consider poor compliance with T4 treatment, pituitary disease & subacute thyroiditis. Consider general health, repeat, possibly check fT3 levels Funny thyroid function tests. Not just funny but bizarre! TSH = 56.2 mu/l, fT4 = 52.6pmol/l. Patient complains of being tired. What would you do? Funny thyroid function tests TSH = 56.2mu/l, fT4 = 52.6pmol/l Consider interference in assay (1:500). Check fT3 or Total T4, anti thyroid abs, use clinical judgement and ask for another lab to perform the assay. TSH levels in TSH-omas are usually much lower. Thyroid Disease in Pregnancy Hypothyroid: check TFTs before planned pregnancy, when pregnancy is diagnosed and expect to increase dose early in pregnancy. Aim TSH > 2 mu/l. Thyrotoxicosis: strict control needed, propylthiouracil preferred, anti receptor antibodies useful in late pregnancy. Early Hyperparathyroidism Consensus guidelines from the Endocrine Society and NIH .(up dated 2009) Surgery remains the mainstay of management for primary HPT. Medical treatment: Vitamin D if low. Biphosphonates ? Cinacalcet possibly. Early Hyperparathyroidism Surgery recommended if serum adjusted Ca > 0.25mmol/l above ULN (=2.8mmol/l). Other Indications for surgery: Hypercalciuria (>10.0mmol/24hr). Age < 50 yrs. Osteopaenia. Serum Creatinine >100umol/l. Not able to be followed up. Trials in Early Hyperparathyroidism. USA -15 yr follow up; (n=49). Baseline serum Ca = 2.62mmol/l 5 year serum Ca = 2.67mmol/l 10 year serum Ca = 2.70mmol/l 15 year serum Ca = 2.78mmol/l (mean serum PTH, serum Creatinine, & 24hr Ur Calcium unchanged). Approx 25% will progress to surgery in 5 yrs. Surgery in Hyperparathyroidism Diagnosis must be confirmed. >95% cure with minimal mordidity. Cheaper after 7 yrs (US). Reduced serum & urine Ca, improved BMD and possible improved QOL. (for higher Ca Levels) Serum Ca & PTH are risk factors for CVD Hypertensive HPT patients at especial risk Glucose intolerance linked to HPT. Early Hyperparathyroidism Follow up of cases where surgery not indicated: Serum Ca & Symptoms – 6 monthly. Serum Creatinine – yearly. Bone density – 2-3 yearly. Vitamin D Deficiency in Adults. Se 25 OH Vit D (nmol/l). <25 25-50 Condition Management Risk of osteomalacia High dose calciferol(10,000u od) For 8-12 weeks. Deficiency with associated disease risk Vit D supplementation (1000 u od) >75 Optimal >500 Toxicity Sources of Vitamin D. UK, 50% of population have insufficient levels and 16% severely deficient in Spring. 20-30 mins sun exposure at midday for a fair skinned person in short sleeved shirt, yield 2000u, (UV B, April –October). Oily fish are best source, also egg yolk, margerine,liver and wild mushrooms. Enzyme inducing agents increase risk of deficiency. Disease associated with Vitamin D Deficiency. Osteomalacia (Alk P’ase usually raised) & myalgia. Probably Increased risk of Diabetes T1 & T2. CVD Bowel & Breast Cancer MS Measuring Vitamin D. Routine results are for 25 - 0H cholecalciferol, ½ life 2-3 weeks.Moderately light stable Active calcitriol (1,25 - OH cholecalciferol has short ½ life, is light instable and is related to serum PTH and does not reflect true Vitamin D status. Ergocalciferol refers to related plant sterols. Treating Vitamin D Deficiency Osteomalacia – 10,000u ergocalciferol daily (may be difficult to obtain), or cholecalciferol (special order) 20,000u capsules 3 per week, or Ergocalciferol 100,000u im, (rpt 3/12 & 612). Insufficiency – 1000u daily as calcium and vitamin D tablets, but tolerability is a problem and is Ca desireable? Consider propriety vit D. Alfacalcidol & Cacitriol preferred for renal failure and hypoparathyroidism. Monitor Serum Ca & Alk p’ase. Diabetes & Cancer T2 DM associated with increased risk of cancer, especially pancreas, breast & colon. This may be multifactorial; Obesity Metabolic Syndrome Raised blood Tg, insulin & IGF1 levels Lower with metformin than SU or Insulin. Diabetes & Cancer 2009, 4 Registry based studies confirm higher risk. Germany: Dose dependent risk for insulin, increased risk for glargine v human insulin. UK Health Information Network, confirmed higher risk SU & insulin. Metformin cut risk for pancreatic & colon cancer. Scotland; Increased breast cancer with glargine versus glargine plus other insulins. Sweden; Also more breast cancer on glargine alone. Diabetes & Cancer Do registry review trials have a selection bias? Detimer; no increased risk. Sitagliptin; in animals increased pancreatic duct cell turnover prevented by metformin. Liraglutide; in rodents increased thyroid c cell tumours, not so far in man. Medical aspects of PCOS 2003 Consensus; Diagnosis made on the basis of 2 of these criteria: Polycystic ovaries on imaging, Oligo-ovulation, anovulation, Clinical / biochemical evidence of androgen excess. (serum testosterone usually <5mmol/l) Medical aspects of PCOS . Investigations may depend on presentation, but may include: U/S Serum LH, FSH, Oestradiol, testosterone. Possibly TFTS, 17OH Progesterone, prolactin. Consider BP, blood glucose. Medical management of PCOS Weight loss 5% Anovulation; Metformin. Clomiphene, FSH Hirsutism; Cyproterone (as Dianette?) Eflornithine (Vaniqa) Local treatments.