Fluid Resuscitation
advertisement
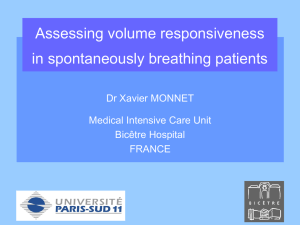
Fluid Resuscitation 2013 NH Benefits Problems Which fluid? Assessing volume status Preload/Volume Status Contractility Afterload/ Vascular tone Predicting Responsiveness Monitoring Response Plan B The setting The environment is bad - time and pressure are monumentally against the considered diagnosis of shock The patient is often bad - More often than not there are multiple comorbidities conspiring to undermine our efforts to maintain homeostasis – small vessel disease, immune dysregulation, Clinical indices of the adequacy of tissue/organ perfusion Mean arterial pressure Cerebral and abdominal perfusion pressures Urine output Mentation Capillary refill Skin perfusion/mottling Cold extremities (and cold knees) Blood lactate Arterial pH, BE and HCO3 Mixed venous oxygen saturation SmvO2 (or ScvO2) Mixed venous pCO2 Tissue pCO2 Skeletal muscle tissue oxygenation (StO2) Aims Ideal Fluid Volume Balance between optimum CO and avoidance of complications (decreased lung compliance, Increased I Abdo pressure, ICP, BP, HR are surrogate markers for CO and have limited correlation VASOPRESSORS Increase afterload Cardiac Output may improve temporarily Potential benefits of fluid administration Preload – haemodynamic parameters Perfusion and oxygenation of organs Brain Heart Kidneys Gut Problems - End Organ damage secondary to resuscitation Lungs – ARDS/ APO Kidneys – ATN Liver – transaminaemia/ impaired gluconeogenesis GUT – Compartment syndrome Brain – Cerebral oedema Fluid volume Only about 50% of patients with circulatory failure will respond to a fluid challenge.[13,16] Important to determine: Preload (LVEDV) Fluid responsiveness, - whether the patient will increase his/her stroke volume or cardiac output with fluid Overall fluid balance - interstitial fluid volume (third space volume). 13. Marik PE, Cavallazzi R, Vasu T, et al. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients. A systematic review of the literature. CritCare Med 2009; 37: 2642–7. 14. Braunwald E, Sonnenblick EH, Ross J. Mechanisms of cardiac contraction and relaxation. In: Braunwald E (ed.).HeartDisease. W.B.Saunders Company: Philadelphia, PA, 1988, pp. 383–425. 15. Nixon JV, Murray RG, Leonard PD, et al. Effect of large variations in preload on left ventricular characteristics in normal subjects. Circulation 1982; 65: 698–703. 16. Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest 2002; 121: 2000–8. Volume Overload Excessive fluid resuscitation with an accumulating positive fluid balance is associated with worse clinical outcomes. Radiographic and clinical signs of pulmonary edema and clinical evidence of peripheral oedema are late signs of volume overload Extravascular lung water (EVLW) as determined by lung ultrasound, transpulmonary thermodilution are two techniques that 'measure' interstitial fluid volume (tissue edema) and may aid in the assessment of volume overload. Vincent JL, Sakr Y, Sprung CL, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 2006; 34: 344–53. Assessing fluid volume status Clinical parameters Preload surrogates: IVC collapsibility CVP Problem = static 60-70% sepsis have cardiac dysfunction CVP responders 8.7 +/- 2.32, non responders 9.7 +/- 2.32 Static Measures: CVP/RAP PCWP LVEDV Dynamic Measures: SBP IVC collapsibility (>20% valid if intubated) >50% valid if non intubated ETC02 - Increase >5% after PLR 75% sens 100% spec for fluid responsiveness (ventilated) Pulse Pressure Variation – ventilated, large Vt etc Stroke Volume (echo) Cardiac Output (Most valid measure) Passive Leg Raise V Fluid challenge Marik CHEST 2008; 134;172-178 ANNALS 2010 March 55(3):290-295 Other techniques: Predictive value of techniques used to determine fluid responsiveness Pulse pressure variation Arterial waveform 0.94 (0.93–0.95) Systolic pressure variation Arterial waveform 0.86 (0.82–0.90) Stroke volume variation Pulse contour analysis 0.84 (0.78–0.88) Left ventricular end-diastolic area Echocardiography 0.64 (0.53–0.74) Global end-diastolic volume Transpulmonary thermodilution 0.56 (0.37–0.67) Central venous pressure Central venous catheter 0.55 (0.18–0.62) *AUC = area under the curve with 95% confidence intervals. nb: Ventilated patients Ref: Hemodynamic Parameters to Guide Fluid Therapy http://www.medscape.com/viewarticle/741748_print Bedside Ultrasound (E-FAST) Good for diagnosing causes of shock: Tamponade RV dilatation ?PE Pneumothorax APO AAA Free fluid in P.O.D ?ectopic Cardiac Output (cardiac probe) Preload You have to fill the tank if its empty.. If CVP v low (1-4) – give fluid >50% change with respiration = CVP<8 >20% change if ventilated Which fluid N Saline Hartmanns Albumin Blood Albumin? Pitfalls Awaiting too long for initiation of vasopressors in patients with overt shock (or awaiting for the patient to be transferred from the ward to ICU to start vasopressors). Slow titration of vasopressors If the patient is persistently hypotensive (i.e., MAP < 65 mm Hg) start vasopressors while continuing IV volume resuscitation It is usually clear within the first 10-15 minutes or less of properly administered IV fluid bolus, whether the blood pressure is properly increasing The washup… Our tools, on the whole, taken in isolation, are fairly appalling for identifying shock. Measures of intravascular volume are all unreliable, particularly in the spontaneously ventilating patient CVP IVC filling on ultrasound Echo lung ultrasound End-tidal carbon dioxide (ETCO2) levels depend on cardiac output. Increasing cardiac output with a fluid challenge or PLR increases ETCO2,as long as ventilatory and metabolic conditions remain stable. In a recent small study, a PLR-induced increase in ETCO2 ≥ 5 % predicted a fluid-induced increase in cardiac index ≥ 15 % with sensitivity of 71 % (95 % confidence interval: 48-89 %) and specificity of 100 (82-100) %(3). The maximal effects of PLR on CI and ETCO2 were observed within 1 min. In summary, differentiating fluid responders from non-responders in the ED remains a challenge. The method used depends on available equipment and expertise, and whether the patient is spontaneously breathing or mechanically ventilated. The NICOM(TM) shows great promise but until your department can afford one, ultrasound is the way to go; small collapsing IVCs suggest fluid responders. Learning to measure a VTI on transthoracic echo or carotid Doppler flow will help you assess the response to a PLR in spontaneously ventilating patients. If they’re mechanically ventilated, then looking for an ETCO2 rise after PLR could be a simpler alternative.