PCOS
advertisement

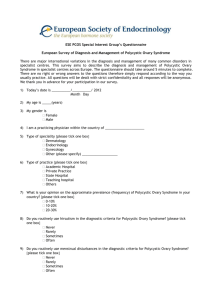
Valerie Robinson, DO • Polycystic Ovarian Syndrome (PCOS) is a disorder that causes menstrual and ovulation irregularities, androgen excess, and infertility. Polycystic ovaries are found on ultrasound. • PCOS is often found in an infertility work-up. • Intraovarian androgen excess excessive growth of small follicles and hinders maturation of a dominant follicle anovulation • Other common findings include obesity and insulin resistance • Prevalence is 6-8% in the general population • Onset is usually during or soon after puberty • Polycystic ovaries may not develop until two or more years after menarche • Increased incidence is found in the following • • • • • • Use of anti-epileptic drugs - specifically valproate Mexican-American First degree family history – risk is 20-40% History of premature adrenarche Diabetes - type 1, type 2, or gestational Infertility • Risk factors • • • • • • First degree relative with polycystic ovaries First degree relative with hyperandrogenism Mother with PCOS Father or Mother with metabolic syndrome Congenital virilization (MCC is congenital adrenal hyperplasia) Insulin resistance or hyperinsulinemia • Menstrual dysfunction • • • • • Oligo- or anovulation Infertility Oligo- or amenorrhea with irregular cycles Adolescents may have delayed menarche May begin regular menses and develop irregularity Increased risk of endometrial hyperplasia/cancer. Oligoovulation results in decreased progesterone secretion. Relative lack of progesterone leads to chronic unopposed estrogen exposure. • Ovarian abnormalities • • • • Multiple small antral and pre-antral follicles in the periphery Follicle growth is arrested in antral stage Increased thickness of stroma Ovarian cortex is thickened and sclerotic • Increased risk of metabolic syndrome • Obesity, usually central • Insulin resistance and hyperinsulinemia • Acanthosis nigricans • Pseudo-acromegaly • Diabetes type 1 or 2 • Dyslipidemia • Hyperandrogenism • Hirsutism • Acne • Male-Pattern balding • Hyperpituitarism • Acromegaly • Hyperprolactinemia • Increased likelihood of depression and anxiety • Increased risk of NASH • Increased risk of CAD • National Institutes of Health (NIH) 1990 criteria: irregular menses, biochemical and/or clinical hyperandrogenism. Other causes of hyperandrogenism excluded. • Rotterdam 2003 criteria (requires two out of three of the following): oligo- and/or anovulation, clinical and/or biochemical hyperandrogenism, polycystic ovaries by ultrasound. Other causes of hyperandrogenism excluded. • Exclude congenital adrenal hyperplasias, androgen-secreting tumors, Cushing's syndrome, hyperprolactinemia, steroid use. • Menstrual history • Physical exam • Transvaginal Ultrasound • 8-10 small follicles surrounding thickened stroma: “String of Pearls” • Rotterdam Criteria: 12 or more follicles 2-9mm, or ovarian volume of >10mL • As a lone finding, polycystic ovaries is insufficient for diagnosis • Hormone abnormalities: non-diagnostic findings • Some women may have increased LH, decreased FSH, increased prolactin • Women with PCOS should be screened for depression, glucose intolerance, dyslipidemia, HTN • Serum HCG to rule out pregnancy in amenorrhea • In high risk women or with virilization, testing may be needed to rule out other uncommon causes of hyperandrogenism. • Morning serum 17-hydroxyprogesterone in the follicular phase • Serum testosterone • Serum prolactin and TSH • Obesity • Weight loss: diet and exercise, bariatric surgery • Insulin-lowering agents: metformin • Hyperandrogenism • Estrogen/Progesterone OCPs, also provide endometrial protection • Antiandrogen after 6 months • Spironolactone (if not planning conception), finasteride • GnRH agonist (leuprolide) suppresses ovarian function • Dyslipidemia • Statins • Fibrates • NASH • Weight loss • Metformin • Anovulation • Weight loss • Clomid • Metformin • Weight loss: • Reduces androgenism, improves ovulation, and increases chance of planned pregnancy. • Insulin-lowering agents • Clomiphine • Increases chances of ovulation • Metformin • Decreases insulin resistance and hyperinsulinemia, increases insulin sensitivity decreased androgens. May promote ovulation • Aromatase inhibitor • Induces ovulation • Gonadotropins – • Increases chances of ovulation • Surgery • We no longer use wedge resection • We do occasionally use “ovarian drilling” to induce ovulation +: usually effective; ±: marginally effective • Ricardo Azziz, MD et al. “Epidemiology and pathogenesis of the polycystic ovary syndrome in adults.” UpToDate. Updated 7/17/12 • Robert L Barbieri, MD, David A Ehrmann, MD et al. “Clinical manifestations of polycystic ovary syndrome in adults.” UpToDate. Updated 8/3/12. • Robert L Barbieri, MD David A Ehrmann, MD et al. “ Diagnosis of polycystic ovary syndrome in adults.” UpToDate. Updated 3/9/12. • Robert L Barbieri, MD David A Ehrmann, MD et al. “Treatment of polycystic ovary syndrome in adults.” UpToDate. Updated 9/20/12. • Robert L Rosenfield, MD et al. “Clinical features and diagnosis of polycystic ovary syndrome in adolescents.” UpToDate. Updated 6/15/11. • Robert L Rosenfield, MD et al. “Definition, pathogenesis, and etiology of polycystic ovary syndrome in adolescents.” UpToDate. Updated 6/15/11. • Robert L Rosenfield, MD et al. “Treatment of polycystic ovary syndrome in adolescents.” UpToDate. Updated 6/16/11. • Figures http://www.advancedfertility.com • Figures https://ufandshands.org/polycystic-ovary-syndrome