Hotspotting in Aurora
Angela Green, PsyD
Heather Logan, MSW
Director of Behavioral Health
Director of Accountable Care & Bridges to Care
Erin Loskutoff, MPH, MSN, AGNP-C
B2C Nurse Practitioner
MCPN
Every touch, every time.
MCPN
Every touch, every time.
MEDICAL REPORT
THE HOTSPOTTERS
Can we lower medical
costs by giving the
neediest patients better
care?
by Atul Gawande JANUARY 24, 2011
The Round Table:
Aligning the Partnerships
What are we trying to accomplish
here?
• Identify WHY patients
over-utilize the hospital:
Build a model around the
WHY
• Stabilize, Coordinate,
Improve Care, Reduce
Cost
• Reduce ER visits and
Inpatient stays through a
community intervention
The Bridges to Care Vision
Helping people one at a
time to empower
themselves with tools,
knowledge, and
confidence to take
responsibility for their
own physical and
psychological health.
Bridges to Care Model
• Hybrid of the Hospital Discharge, ED,
Home, and Community Based Models
• Intervention begins at bedside
• 60 day model: Patient graduates from the
program
• 8 visits minimum
• Collect information at each step to
evaluate/improve program
• Inclusion/Exclusion Criteria
• MCPN’s model includes 2 unique
components
Medical Providers
Behavioral Health Providers
Criteria
INCLUSION
• Live in Aurora
• 3 Hospital Visits (ER & IP) in
last 6 months
• Adults
• Non-violent offenders,
homeless, BH are all ok
EXCLUSION
•
•
•
•
•
•
•
•
•
•
•
Acute visits (?)
Pregnancy
HIV (?)
Malignancies
Primary dx of personality
disorder
Post-surgical
Primary diagnoses of substance
abuse
Diminished capacity
Pediatrics
Violent offenders/sex offenders
Care giver as primary decision
maker or Power of Attorney
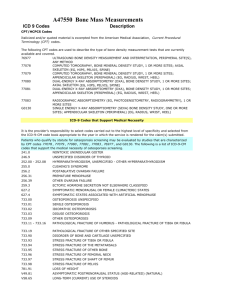
B2C Home Visit Timeline
60 day model (Minimum of 8 visits)
More home visits may be needed to graduate the patient from the program
NOT ALL PATIENTS WILL FOLLOW THIS TIMELINE EXACTLY.
Enrollment 24-72hrs post d/c
CHW/CCC
Pre-Graduation Visit –
HC
Present giveaways and B2C
contact info
Any combination of
NP/BHP/CCC/PNP/
HC
Complete Enrollment forms
Pre-enrollment
#1
#2
#3
Any combination of
NP/BHP/CCC/PNP/
HC
#4
#5
Review graduation
checklist - Teach-back
Opportunities
#6
#7
#8
333333#
Medical Visit w/ NP
Complete pre-enrollment
forms (Track Via) - CHW
Schedule:
1st Home Visit (Enrollment
w/CCC)
2nd Home Visit - NP visit
Updated8/5/13 SA
(w/in a week of
hospital d/c- if
possible)
30 days Assessment
HC
Complete 30 day
assessment and
Outcome forms
Any combination of
NP/BHP/CCC/PNP
/HC
Graduation Celebration –
CCC
Present giveaways and
home clinic contact
information
Complete -60 day
assessment and Outcome
forms
Behavioral Health:
An Essential Component
• SDAC data revealed nearly 80% of Medicaid
patients in this data set had a behavioral
health component to condition
AIM-C Approach
• Assess – SBIRT, PHQ, initial visit,
CPCQ, risk stratification, enrollment
evaluation, CCC assessment
• Intervene – brief counseling, meds,
referrals, coaching
• EMpower – educate, activate,
validate, participate, motivate
• Connect – relationship, resources,
referrals
Outcomes/Deliverables
• 1. Enroll our 689 patients
• 2. Demonstrate cost savings
•
- Reduce re-hospitalizations
•
- Decrease Illness Burden
• 3. Transition patients from home visits to clinic
visits
• 4. Establish health homes for patients
• 5. Demonstrate sustainability/develop a
sustainability plan
Demographics
Demographics
Demographics
Transitional
1%
B2C Homeless Status
Unknown
1%
Street
2%
Other
21%
Doublin
g Up
7%
Not Homeless
54%
Homeless
Shelter
1%
None
13%
Encounters By Type & Team Member
Encounters by Type & Provider
MA
6%
BH
4%
Psych NP
5%
CHW
26%
Health Coach
15%
Med
16%
CCC
28%
Physically Unhealthy Days
120
107
100
94
80
80%
71%
65
60
49%
40
38
30
29%
23
23%
20
17%
16
14
12%
11%
12
12%
0
After 30 days
After 60 Days
Increase
Unchanged
After 180 days
Decrease
N = 133
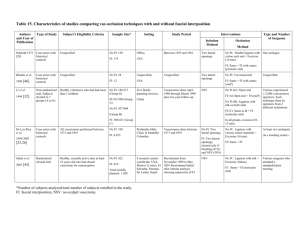
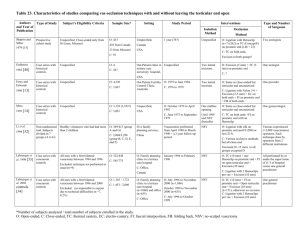
Chronic Diagnoses
B2C Status
Active
Graduated
Lost to Follow
Total
•
More than 1 Chronic DX
36
239
83
358
Frequency
38
244
106
388
Percentage
95%
98%
78%
92%
An overwhelming proportion of B2C patients suffer from chronic illnesses (92%)
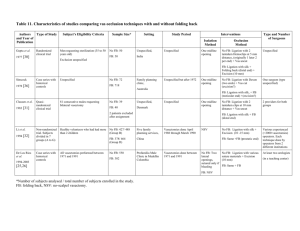
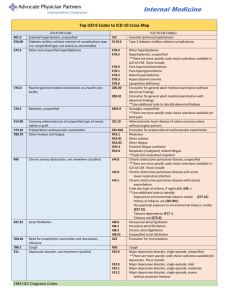
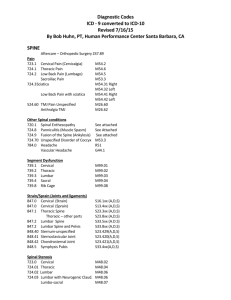
Top 20 Chronic Diagnoses (All statuses)
1
2
3
4
5
6
7
8
9
ICD9
401.9
305.1
311
300.00
250.00
272.4
493.90
300.4
530.81
Description
Unspecified essential hypertension
Nondependent tobacco use disorder
Depressive disorder, not elsewhere classified
Anxiety state, unspecified
Diabetes mellitus without mention of complication, type II or unspecified type, not stated as uncontrolled
Other and unspecified hyperlipidemia
Asthma, unspecified, unspecified
Dysthymic disorder
Esophageal reflux
Freq
183
141
103
95
90
88
79
60
58
10
278.00
Obesity, unspecified
56
11
309.81
Posttraumatic stress disorder C
50
12
250.02
Diabetes mellitus without mention of complication, type II or unspecified type, uncontrolled
42
13
496
Chronic airway obstruction, not elsewhere classified
40
14
300.01
Panic disorder without agoraphobia
38
15
296.80
Bipolar disorder, unspecified
37
16
244.9
Unspecified hypothyroidism
36
17
428.0
Congestive heart failure, unspecified
33
18
305.00
Nondependent alcohol abuse, unspecified drunkenness
31
19
296.32
Major depressive disorder, recurrent episode, moderate
28
20
346.90
Unspecified migraine without mention of intractable migraine
27
B2C Patients with BH Diagnoses
78% of Active patients
86 % of Graduates
81% of All B2C Patients
69% of Lost to Follow
90
Mentally Unhealthy Days
79
80
70
70
63
60
59%
53%
50
47%
40
39
37
33
33
30
30
25%
29%
28%
25%
20
23%
15
11%
10
0
After 30 days
After 60 Days
Increase
Unchanged
After 180 days
Decrease
N = 133
Current B2C – Utilization Trend Data
Current B2C – Utilization Trend Data
What We Already Know
About Cost Savings
“Health centers save $1,263 per
person per year, lowering costs across
the delivery system‒from ambulatory
care settings to the emergency
department to hospital stays”
Source: NACHC analysis based on Ku L et al. Using Primary Care to Bend the Curve: Estimating the Impact of
a Health Center Expansion on Health Care Costs.
GWU Department of Health Policy. Policy Research Brief No. 14. September 2009.
Lessons Learned
•
•
•
•
•
•
You need good people to do hard work!
Systems are not designed for innovative work!
Chances are no one has gotten this far before!
Sometimes being a gardner is all you can do!
Be realistic about what change means!
Buy in is crucial, it just may not always come
from the top or look the way you envisioned!
Constantly Evolving: Don’t use pen!
Achieving the Triple Aim
“The integrator’s role includes
at least five components:
1. Partnership with individuals
and families,
2. Redesign of primary care,
3. Population health
management,
4. Financial management, and
5. Macro system integration. “
Health Aff May 2008 vol. 27 no. 3 759-769
Thank you.