Biting Flies - PHSource.us
advertisement

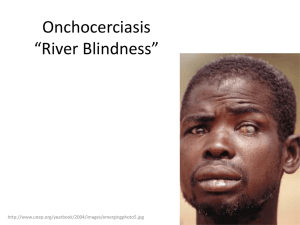
Other Biting Flies Blackflies, Biting Midges, Tabanid Flies, and Sandflies Associated Pathogens, Life Cycles, Vector Biology and Control 1 Blackflies and Onchocerciasis • Pathogens • Life Cycles • Vector Biology • Vector Control 2 3 Onchocerciasis • • • • Non-fatal dermal and ocular disease Human definitive host; fly intermediate host No animal reservoir of O. volvulus 95% of all cases worldwide occur in Africa in poor rural areas, approx. 17 million affected • Three main symptoms (occur 1-3 yrs after initial infection): • Skin lesions (microfilariae in dermis) • Painless nodules (where tissues thin, bone) • Eye lesions (blindness – assoc. with dead mf) 4 5 Onchocerca life cycle - 1 • During a blood meal, an infected blackfly (genus Simulium) introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound. • In subcutaneous tissues the larvae develop into adult filariae, which commonly reside in nodules in subcutaneous connective tissues. • Adults can live in the nodules for approximately 15 years. Some nodules may contain numerous male and female worms. • Females measure 33 to 50 cm in length and 270 to 400 µm in diameter, while males measure 19 to 42 mm by 130 to 210 µm. • In the subcutaneous nodules, the female worms are capable 6 of producing microfilariae for approximately 9 years. Onchocerca life cycle - 2 • The microfilariae, measuring 220 to 360 µm by 5 to 9 µm and unsheathed, have a life span that may reach 2 years. • They are occasionally found in peripheral blood, urine, and sputum but are typically found in the skin and in the lymphatics of connective tissues. • A blackfly ingests the microfilariae during a blood meal. • After ingestion, the microfilariae migrate from the blackfly's midgut through the hemocoel to the thoracic muscles. • There the microfilariae develop into first-stage larvae and subsequently into third-stage infective larvae. • The third-stage infective larvae migrate to the blackfly's proboscis and can infect another human when the fly takes 7 a blood meal. Onchocerciasis is endemic in more than 25 nations located in a broad band across the central part of Africa. Small endemic foci are also present in the Arabian Peninsula (Yemen) and in the Americas (Brazil, Colombia, Ecuador, 8 Guatemala, southern Mexico, and Venezuela). © Copyright 1997 OCP/APOC/WHO. Adults of Onchocerca volvulus from nodule. 9 Microfilaria of Onchocerca volvulus, from skin snip from a patient seen in Guatemala. Wet preparation. Some important characteristics of the microfilariae of this species are shown here: no sheath present; the tail is tapered and is sharply angled at the end. 10 © Copyright 1997 OCP/APOC/WHO. Blindness caused by onchocerciasis 11 © Copyright 1997 OCP/APOC/WHO. Maddening itching, depigmentation (leopard skin), and thickened skin 12 13 14 Eggs of Simulium damnosum attached to vegetation in running water. Adults typically emerge in 8-12 days, depending on local temperature. 15 Larva Simulium naevei larvae attached to a crab. Pupae 16 West Africa, 1990, WHO/TDR Guatemala, 1991, WHO/TDR/Haaland Simulium damnosum larvae. Blackfly larvae and pupae found during a survey of a stream near Los Golindras, 3 hours drive north of Huixla, Guatemala. 17 Collecting blackfly immatures Single blackfly larva and larvae clustered on a stick in moving 18 water Nigeria, Africa, 1998, WHO/TDR/Crump Uganda, Africa, 1996 WHO/TDR/Crump The Simulium blackfly vectors breed in fast-flowing river water such as this, and threaten those farming fertile riverside land with infection and blindness. Fast-flowing waters in rivers are ideal breeding sites for the blackfly. 19 Ghana, Africa, 1973 WHO/TDR/Baldry A breeding site for Simulium damnosum the blackfly vector of Onchocerca volvulus. Human activities can sometimes create the conditions sought by blackflies for breeding. 20 21 22 West Africa, 1990 WHO/TDR/W. Imber Adult Simulium damnosum taking a bloodmeal – only females take blood and may live up to 4 weeks 23 24 Onchocerciasis Control Vector Control - The principal method for controlling onchocerciasis has been to break the cycle of transmission by eliminating the black fly. Simulium larvae are destroyed by application of selected insecticides through aerial spraying of breeding sites in fast-flowing rivers. Once the cycle of river blindness has been interrupted for 14 years the reservoir of adult worms dies out in the human population, thus eliminating the source of the disease. Ivermectin Treatment - To complement vector control activities, the drug ivermectin is distributed where needed through a community directed approach. Ivermectin kills the larval worms that cause blindness and other onchocercal manifestations and acts to decrease transmission as well. Ivermectin became available in 1987 to complement blackfly control activities. 25 Treatment (CDC Recs) • Use of antibacterial cream on wounds stops bacterial infections and keeps swelling from worsening. • Diethylcarbamazine (under an investigational New Drug Protocol from CDC's Drug Service) and ivermectin* are effective for the treatment of filariasis. • Albendazole* is also included among the choices for treatment of filariasis. * This drug is approved by the FDA, but considered investigational for this purpose. 26 DRUG MODE OF ACTION • Ivermectin (Mectizan®)- binds to glutamate gated chloride channels in the parasites’ nervous system, causing them to open. • Albendazole - works by keeping the worm from absorbing sugar (glucose), so that the worm loses energy and dies. • Diethylcarbamazine – causes hyperpolarization of nerve membrane and flaccid paralysis of the nematode, worms are removed by normal peristalsis 27 Onchocerciasis Control Programme in West Africa (1974-2002) The Onchocerciasis Control Programme in West Africa (OCP) has brought onchocerciasis under control in the savanna areas of 11 West African countries where the disease used to be a major public health problem and a serious obstacle to socio-economic development. The current challenge of OCP, which ended in the year 2002, is to ensure that its achievements can be maintained by the countries themselves. 28 Microfilarial Prevalence 20 Years Later Pre-Control Microfilarial Prevalence 29 The African Programme for Onchocerciasis Control (APOC) covers 19 African countries and more than 85% of all people affected by onchocerciasis, or river blindness, in the world. With the goal of elimination of river blindness as a public health and socioeconomic problem throughout Africa, APOC intends to establish selfsustainable communitydirected treatment with ivermectin throughout the endemic areas and to eradicate the vector in selected foci. African Programme for Onchocerciasis Control 30 Existing oncho foci in the Americas Onchocerciasis Elimination Program in the Americas (OEPA) To coordinate onchocerciasis control efforts in the 6 endemic countries of the Americas and to reach the goal of eliminating first the pathology and then the disease, the Onchocerciasis Elimination Programme for the Americas (OEPA) was created in 1992 with the support of PAHO, the Inter-American Development Bank, a consortium of NGDOs, and all of the affected countries. 31 Mali, Africa, 1996, WHO/TDR/Crump Mali, Africa, 1996, WHO/TDR/Crump Flies collected during Man-bait capture and essential tools for Man-bait capture. A volunteer sits by a fast-flowing part of a river where the Simulium blackfly vectors breed. Flies which land on him are collected32in tubes, labeled and then dissected to see if they are carrying parasites. © Copyright 1997 OCP/APOC/WHO. Vector collectors catch the Simulium fly as it lands on the legs to take up a blood meal through its bite. 33 Mali, Africa, 1996, WHO/TDR/Crump Man-bait capture. Flies which land on the volunteer are collected in tubes, labeled and then dissected to see if they are carrying parasites. 34 West Africa, 1990, WHO/TDR/OCP/Ward As part of the Onchocerciasis Control Programme (OCP), helicopters and fixed wing aircraft are used to spray insecticides (chemical and biological) on rivers and fastflowing water where larvae of the blackfly, Simulium damnosum, breed. Insecticide types used are organophosphates, carbamates and pyrethroids. 35 West Africa, 1990, WHO/TDR/OCP/Ward Seven insecticides are currently available to the Program: Bti, Abate, pyraclofos, phoxim, permethrin, carbosulfan and vectron. They are used on a rotational basis depending on the river disharge, the level of toxicity with respect to non-target organisms and the level of sensitivity of the local Simulium species to each of the compounds. 36 New villages in areas formerly uninhabitable because of river blindness The result has been increased activity and productivity in many 37 of these areas Nine million children born after 1974 have been saved from river blindness Formerly empty schools have reopened their doors 38 Mansonella ozzardi 39 • M. ozzardi consists of two biological forms. Mansonella ozzardi distribution • One is transmitted by black flies of the Simulium family and is mainly found in the Amazon and parts of the South American mainland. • The other form is transmitted by midges of the Culicoides family and is endemic to beach areas in the Caribbean where these pests are common. 40 Mansonella ozzardi • Once in the human host the larvae move into the peritoneal cavities. • The adults then mate and produce unsheathed microfilariae about 207-232 x 3-4 micrometers in size. • The microfilaria closely resemble those of M. perstans except they have a sharp tail. • They are non-periodic like their vectors and can be found in the blood and skin at all times. • Most infected people are completely symptomless. • However, joint pains, headaches, coldness of the legs, inguinal adenitis, and itchy red spots have been described in conjunction with infection. 41 42 Summary - Blackflies • Pathogens • Life Cycles • Vector Biology • Vector and Disease Control 43 Other Bloodsucking Flies Associated with Filarial Transmission Vector Biology and Pathogen Transmission • Culicoides sp. (Biting Midges) • Tabanidae (Horse flies and Deer flies) 44 Biting Midges – Medical Importance • PEST impact – tourism, economics • Mansonella perstans and M. streptocerca (filarids) transmitted by Culicoides sp. In Africa • M. ozzardi transmitted by C. furens in S. & C. America • Filariae develop in thoracic flight muscles • Oropoche virus (Brazil, Trinidad and Colombia) • Blue tongue virus (cattle, sheep – vet. importance) 45 46 • Mansonella perstans occurs in both Africa and South America • Infections by Mansonella perstans, while often asymptomatic, can be associated with angioedema, pruritus, fever, headaches, arthralgias, and neurologic manifestations. 47 48 • Mansonella streptocerca is found in Africa • Mansonella streptocerca can cause skin manifestations including pruritus, papular eruptions and pigmentation changes. 49 • May be transmitted by midges of the Culicoides family and is endemic to beach areas in the Caribbean where these pests are common. Mansonella ozzardi distribution • Most infected people are completely asymptomatic. However, joint pains, headaches, coldness of the legs, inguinal adenitis, and itchy red spots have been described in conjunction with infection. 50 51 Culicoides larva 52 Biting Midges Culicoides pupae and adult 53 Culicoides habitat – many larval habitats similar to that of mosquitoes 54 Family Tabanidae – Medical Importance • Large biting flies in two genera – Tabanus, Chrysops • Tabanus sp. – horseflies (tularemia) • Chrysops sp. – deerflies (Loa loa, tularemia) • Filariae develop in fat body of thorax and abdomen • Large biting mouthparts, pool feeders (females only) • Usually diurnal activity, powerful fliers 55 56 57 • The vectors for Loa loa filariasis are flies from two species of the genus Chrysops, C. silacea and C. dimidiata. Loiasis only occurs in Africa and infection is often asymptomatic. • During a blood meal, an infected fly (genus Chrysops, daybiting flies) introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound . • The larvae develop into adults that commonly reside in subcutaneous tissue . • Adults produce microfilariae measuring 250 to 300 µm by 6 to 8 µm, which are sheathed and have diurnal periodicity. • Microfilariae have been recovered from spinal fluids, urine, and sputum. During the day they are found in peripheral blood, but during the noncirculation phase, they are found in the lungs . 58 59 60 61 62 63 Tabanid Teeth Serrated edges usually associated with bloodfeeding species. 64 65 66 67 Deer flies feeding 68 Summary - Bloodsucking Flies Associated with Filarial Transmission • Culicoides sp. (Biting Midges) • Tabanidae (Horse flies and Deer flies) 69 Other Bloodsucking Flies: Sandflies and Leishmania Vector Biology and Pathogen Transmission 70 Sandflies – Medical Importance • Small biting flies in two genera – Phlebotomus (Old World), Lutzomyia (New World) • Transmit leishmaniasis (worldwide) • Transmit sandfly fever virus (Mediterranean) • Transmit Carrion’s disease (bartonellosis) Peru, Ecuador and Columbia 71 LEISHMANIASIS • Caused by obligate intracellular protozoa of the genus Leishmania. • Human infection is caused by about 21 of 30 species that infect mammals. • These include the L. donovani complex with 3 species (L. donovani, L. infantum, and L. chagasi); the L. mexicana complex with 3 main species (L. mexicana, L. amazonensis, and L. venezuelensis); L. tropica; L. major; L. aethiopica; and the subgenus Viannia with 4 main species (L. (V.) braziliensis, L. (V.) guyanensis, L. (V.) panamensis, and L. (V.) peruviana). • The different species are morphologically indistinguishable, but they can be differentiated by isoenzyme analysis, molecular methods, or monoclonal antibodies. 72 During bloodfeeding, female sandflies inject the infective promastigote stage. Promastigotes that reach the puncture wound are phagocytized by macrophages and transform into amastigotes. Amastigotes multiply in infected cells and affect different tissues, depending in part on the Leishmania species. This originates the clinical manifestations of 73 leishmaniasis. Sandflies become infected during blood meals on an infected host when they ingest macrophages infected with amastigotes. In the sandfly's midgut, the parasites differentiate into promastigotes, which multiply and migrate to the 74 proboscis. Leishmania donovani promastigotes (form present in sandfly host) 75 Leishmania donovani extracellular amastigote (form present in vertebrate host) 76 LEISHMANIASIS - manifestations • Human leishmanial infections can result in 2 main forms of disease, cutaneous leishmaniasis (CL) and visceral leishmaniasis (VL) (also known as kala-azar). • Two less common forms also occur: mucocutaneous leishmaniasis (MCL), due to L. braziliensis infection, and diffuse cutaneous leishmaniasis (DCL), which produces disseminated and chronic skin lesions. • The factors determining the form of disease include leishmanial species, geographic location, and immune response of the host. 77 LEISHMANIASIS - pathology Cutaneous forms of the disease normally produce skin ulcers on the exposed parts of the body such as the face, arms and legs. The disease can produce a large number of lesions sometimes up to 200 - causing serious disability and leaving the patient permanently scarred. In mucocutaneous forms of leishmaniasis , lesions can lead to partial or total destruction of the mucose membranes of the nose, mouth and throat cavities and surrounding tissues. Visceral leishmaniasis - also known as kala azar - is characterized by irregular bouts of fever, substantial weight loss, swelling of the spleen and liver, and anemia (occasionally serious). If left untreated, the fatality rate can be as high as 100%. 78 Leishmaniasis – Cause and Effect • Leishmaniasis is related to environmental changes such as deforestation, building of dams, new irrigation schemes, urbanization and migration of non-immune people to endemic areas. • It seriously hampers productivity and socioeconomic progress and epidemics have significantly delayed the implementation of numerous development programs. • This is particularly true in Saudi Arabia, Morocco, the Amazon basin and the tropical regions of the Andean countries. 79 Currently the leishmaniases, prevalent in four continents, are considered to be endemic in 88 countries, 72 of which are developing countries: • 90% of all visceral leishmaniasis cases occur in Bangladesh, Brazil, India, Nepal and the Sudan • 90% of mucocutaneous leishmaniasis occurs in Bolivia, Brazil and Peru • 90% of cutaneous leishmaniasis cases occur in Afghanistan, Brazil, Iran, Peru, Saudi Arabia and Syria 80 81 Leishmania/HIV co-infection • Leishmaniasis is spreading in several areas of the world as a result of epidemiological changes which sharply increase the overlapping of AIDS and visceral leishmaniasis. • So far, 33 countries worldwide have reported coinfections. • Intravenous drug users have been identified as the main population at risk. 82 83 84 85 TREATMENT Andy Crump WHO/TDR/Crump A tube of paromomycin cream, used for topical application on lesions in the treatment of cutaneous leishmaniasis A doctor filling a syringe from a phial of glucantime, a pentavalent antimonial which is used for the treatment of cutaneous leishmaniasis 86 Cutaneous Leishmaniasis 87 Diffuse Cutaneous Leishmaniasis 88 89 TREATMENT Andy Crump WHO/TDR/Crump A bottle of capsules of miltefosine, the first oral drug for treating visceral leishmaniasis. A number of clinical studies to test the effectiveness of injectable paromomycin against visceral leishmaniasis have been carried out in India, where the standard antimonial treatment, sodium stibogluconate, is not very effective and failure rates are high. Results show it to be safe and effective. 90 SANDFLIES • Worldwide distribution • 700 species in 5 genera (Family Psychodidae, subfamily Phlebotominae) • Three genera contain bloodsucking species • Most important genera are Phlebotomus (Old World) and Lutzomyia (New World) 91 Important Vectors of Leishmaniasis Visceral Lutzomyia longipalpis Central and South America Phlebotomus argentipes Middle East Phlebotomus chinensis China Cutaneous Phlebotomus sergenti India Phlebotomus papatasi Mediterranean Lutzomyia verrucarum s.l. Central and South America Mucocutaneous Lutzomyia intermedia http://cipa.snv.jussieu.fr/index.html Central and South America 92 93 Sandfly Pupa 94 Sandfly Larvae 95 SANDFLIES: Adults • Differentiate between Phlebotomus and Lutzomyia by where (geographically) they are collected • Very small (1.3-3.5 mm), very hairy, with long thin legs • Body tends to be brown/light brown in color • Short mouthparts adapted for sucking – only females take blood, usually nocturnal • Wings held over the body when at rest – generally poor fliers 96 97 WHO/TDR/Stammers Lutzomyia longipalpis feeding 98 WHO/TDR/Stammers Phlebotomus duboscqi feeding 99 100 Dogs can act as reservoirs of Leishmania parasites. They also exhibit symptoms of infection. 101 WHO/TDR/Mark Edwards Rodent reservoir hosts WHO/TDR/Crump Rodent burrows 102 WHO/TDR/Lainson Rubber trees in part of a natural, uncut forest which is a locality for the transmission of leishmaniasis (Espundia) in Brazil. People who collect rubber in these situations, or who clear such areas for agricultural use, are prone to infection. 103 WHO/TDR/Mark Edwards Rio de Janeiro. Homes built in newly-cleared forest areas around the city perimeter, in transmission sites such as the Fragrasia Mountains, expose the settlers to the sandflies 104 which transmit leishmaniasis. WHO/TDR/Mark Edwards Sandfly habitat in Jacarepagua district on the outskirts of Rio de Janeiro. Homes built in newly-cleared forest areas expose the 105 settlers to the sandflies which transmit leishmaniasis. Vector Control Bednet protection from sand flies 106 Spraying to control sand flies 107 Summary - Biting Flies (Other than Mosquitoes) • Blackflies – Onchocera, Mansonella • Biting Midges – Mansonella • Tabanid Flies: • Deer flies – Loa loa, tularemia • Horse flies - tularemia • Sandflies – Leishmania, sandfly fever virus, bartonellosis 108