current status of health information system: indonesia
advertisement
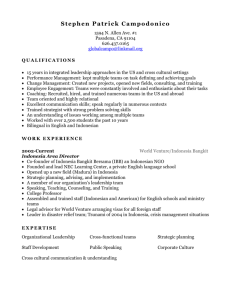
CURRENT STATUS OF HEALTH INFORMATION SYSTEM: INDONESIA* Soewarta Kosen National Institute of Health Research & Development Center for Community Empowerment, Health Policy and Humanities Jakarta, Indonesia Presented at the 6th Meeting of the Asia Pacific Network of the WHO IFC, Bangkok, Thailand, 18-19 July 2013 BACKGROUND Law No 36/2009 on Health states that to manage effective and efficient health efforts, health information is needed and should be implemented through the health information system and include information from other sectors To be optimum, the Health Information System needs cooperation and support of various sectors and cover integrated information from health sector and all other health related sectors for policy formulation Law No 23/2006 on Population Administration stated that Vital Registration is implemented through Population Administration Information System from village/kelurahan up to district, city, province and national BACKGROUND Sources of Health Information System and basic demographic statistics in Indonesia include: population administration information system (Civil Registration), Population Census, National Socioeconomic Survey, Demographic Health Survey, National Health Survey, Baseline Health Research (RisKesDas), regular recording-reporting system of Puskesmas (Community Health Center) and Hospitals, surveillance data, sentinel data: Nutrition, MCH, Family Planning, Mortality Data with Multiple Causes of Death (ICD – 10) The benefits of a well-developed information system include the ability to monitor impact of health programs, better quality information, and more efficient delivery of health care services. With sound data sources and proper data collection, transforming data and information (evidence) into policy becomes best practices Health Information Data Sources Civil Registration Service Records Population Surveys Community Individual Records Population based Facility based Processing & Integrating data Census Resource Records Saving of Integrated data Integrated Health Information System Sources of Data MonitEvaluation: reports, event inquiries & warning Fact & evidence from HIS, used for decision making • MoH • Other gov’t ministries • Local health offices (prov/ district/city) • International agencies • Universities • Researchers • etc. Standardized Data Collection POLICY, RESOURCES AND PROCESS Source: HMN, 2008 CHARACTERISTICS OF THE INDONESIAN HEALTH INFORMATION SYSTEM The HIS includes data of health sector & other related development sectors (FP, Social Welfare, Agriculture) The HIS integrates routine facility based data and nonroutine community based data (survey, census): Baseline Health Research, Facility Based Survey, Demographic Health Survey, National Socio-economic Survey Used for advocacy, program planning, monitoring and management; as well as for evaluation Emphasize: availability, quality, value & utilization of timely and accurate information TYPE OF COLLECTED DATA IN HIS Health status (morbidity, disability and mortality) Health efforts (public goods & private goods) Health care financing Health man-power Drugs and supplies Community empowerment in health Health resources: building/physical infrastructure, medical equipment and non-medical (vehicles, furnitures) Local specific data CHARACTERISTICS OF IMPROVED INDONESIAN HIS Self reliance Data & information are processed and analyzed mainly at and for local use (operational level) Applying conventional (paper based) as well as ICT/computer based procedures: maximize efficiency (personnel time) and effectiveness (relevance & usefulness) Proper selection of essential indicators: Obligatory Public Health Functions/Minimum Service Standard; to serve the need of data and information at various levels, including local level (city, district, prov.) Development of a network of data-bank Comprehensive & relevant for health development N CURRENT ACHIEVEMENT OF INDONESIAN CRVS W E S Uses of e-ID & unique population number in all over Indonesia: accelerate better civil registration (births, deaths) and causes of death Several cities & districts have allocated special budget for CRVS activities Joined efforts (MoH & MoHA) to improve Civil Registration and certification of causes of death based on existing law and regulations, use the information for national and local planning and policy formulation Collection of real-time of vital statistics data and causes of death, through Sample Registration System SITUATIONAL ANALYSIS Identified weakness of Indonesian HIS: ◦ ◦ ◦ ◦ ◦ Irrelevance of the collected information Fragmented & poor quality of data Duplication among parallel information Lack of timely reporting and feedback Minimal analysis and use of data & information at local level (district and city) for advocacy, program planning, monitoring and management; as well as for obtaining needed resources STATISTICS BASED ON WHO - FIC Provide basic information to formulate policies, priorities and development of intervention programs (health and non health) as well as a guidance in allocating resources As a base to monitor and evaluate program effectiveness of basic services/obligatory public health functions, their achievements and trends To determine research priorities, e.g. relationship of tobacco and certain diseases, causes of high incidence of stroke, determine risk factors, relationship with socioeconomic level, demography and behavior INDONESIAN SAMPLE REGISTRATION SYSTEM (SRS) Indonesian SRS sites cover 128 Sub-Districts in 89 districts and 25 cities (7 regions and 30 provinces) that represent Indonesia Total population covered about 4 % of Total Population (240 millions): about 9 millions to represent Indonesia Stratified into Development Area (7) and Urban - Rural Joint Decree of the Minister of Home Affairs and the Minister of Health (January 2010) on Reporting of Death and Cause of Death facilitates the recording of events and cooperation between the two sectors at the grass-root level COMPONENTS OF THE WHO VERBAL AUTOPSY GUIDELINES I. Questionnaire for interview with family members and/or caregivers Standard questionnaires permit reasonably accurate ascertainment of causes of death based on responses to a well-administered questionnaire. Responses to questionnaire analysed for classification and coding in line with ICD-10 II. Application of ICD-10 to verbal autopsy interviews Certification by medically trained personnel Professionalised coding ICF (INTERNATIONAL CLASSIFICATION OF FUNCTIONING, DISABILITY AND HEALTH), WHO 2001 Collected thru Baseline Health Research 2007 and 2013 for situational analysis of disabilities Applied in Disability Weight Survey for Global Burden of Disease 2010 (3 provinces of Indonesia) Indonesia Statistical Office incorporates the ICF Concept for Handicapped Survey (together with the Ministry of Social Affairs) CONCLUSIONS Need to emphasize the Medical Certification of Cause of Death (MCCD) as a confidential part of the formal death certificate Need to refresh medical communities (physicians) in all health facilities (hospitals and community health centers) on the writing of multiple causes of death based on ICD – 10 Need to enforce compulsory mortality registration based on current national law & regulations and support the formulation of local regulations Since the majority of deaths occur outside the hospital, verbal autopsy method to obtain causes of death has to be disseminated and carried out for deaths occurring in the community Accelerate development of ICT to assure more reliable, timely and complete Health Information System CONCLUSIONS The improved Indonesian Health Information System based on WHO - Family International Classification: Be adaptive to the information need of the health sector, relevant and produce better quality of data to support planning and management at various levels of administration Permit development of integrated and comprehensive HIS to support the national and local health systems Be locally sustainable Be able to monitor achievement in health development, including Medium Term National Health Dev’t Plan, MDGs, WSC , etc. ULTIMATE TARGET: Disseminate information culture: “no reasons to make decisions without information and evidence based support” TERIMA KASIH