Clinical Education: Competencies and Conversations
advertisement
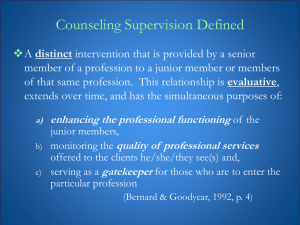
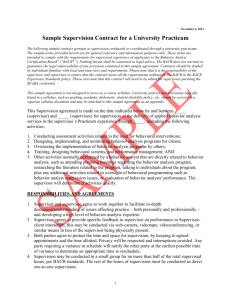
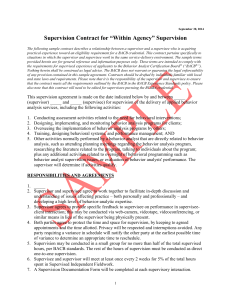
Clinical Education: Competencies and Conversations KSHA 2012 KSHA 2012 Outline • Background Information – Standards for Clinical Education – Competency Based Outcomes; Knowledge and Skills Needed by SLPs Providing Clinical Education– Debby Daniels, KUMC • Strategies for Collaborative Teaching and Learning – A Continuum of Support – Melanie Hilgers, KSU – Clinical Educator: Strategies to Promote Learning – Jane Wegner, KU – Active Engagement on the Part of the Student – Marla Staab, FHSU – The Art of Giving Feedback – Laurie Hughey, WSU • Discussion; scenarios Standards for Accreditation – Clinical Education • Council on Academic Accreditation (CAA) in Audiology and Speech-Language Pathology of ASHA – Sets and implements standards – Awards accreditation Standards for Accreditation – Clinical Education • Six necessary components for quality graduate education – Administrative structure and governance – Faculty – Curriculum (academic and clinical education) – Students – Assessment – Program resources Standards for Accreditation – Clinical Education • Standard 3.1B – The curriculum (academic and clinical education) is consistent with the mission and goals of the program and prepares students in the full breadth and depth in the scope of practice in speechlanguage pathology. Standards for Accreditation – Clinical Education • Program curriculum must provide opportunity for students to obtain – A minimum of 400 supervised clinical education hours, of which 325 must be attained at the graduate level – Provide sufficient breadth and depth of opportunities to gain experiences with • Different work settings • Different populations • Appropriate equipment and resources Standards for Accreditation – Clinical Education • The program must provide opportunities for students to acquire and demonstrate knowledge & skills in – – – – – – – – Articulation Fluency Receptive/expressive language Hearing Swallowing Cognitive aspects of communication Social aspects of communication Communication modalities Standards for Accreditation – Clinical Education • The program must provide opportunities for students to acquire and demonstrate knowledge & skills in – Oral and written or other forms of communication – Prevention, evaluation and intervention of communication and swallowing disorders – Interaction, including counseling and collaboration – Effective interactions – Delivery of services to culturally and linguistically diverse populations – Application of the principles of evidence-based practices – Self-evaluation of effectiveness of clinical practice Standards for Accreditation – Clinical Education • Clinical supervision is commensurate with the clinical knowledge and skills of each student, and clinical procedures ensure the welfare of each person served by students is protected, in accord with recognized standards of ethical practice and relevant federal and state regulations. How Much Supervision????? • Standard IV-E of SLP Certification Handbook – Direct supervision must be in real time and never be less than 25% of the student’s total contact with each client/patient and must take place periodically within the practicum. These are minimum experiences that should be adjusted upward if the student’s level of knowledge, experience, and competence warrants. Standards for Accreditation – Clinical Education • Written policies describing the manner and amount of supervision • Written procedures for client/patient safety, confidentiality, and security of client/patient records Standards for Accreditation – Student Assessment • Competency Based Outcomes – Formative Assessments – Summative Assessments Clinical Supervision Competencies • http://www.asha.org/docs/html/PS198500220.html – Tasks of supervision – Competencies for effective clinical supervision – Preparation of clinical supervisors Tasks & Competencies of Supervision • Establishing and maintaining effective working relationship with supervisee • Assisting supervisee in developing clinical skills and objectives • Assisting the supervisee in developing and refining assessment skills • Assisting the supervisee in developing and refining clinical management skills • Demonstrating for and participating with the supervisee in the clinical process • Assisting the supervisee in observing and analyzing assessment and treatment sessions Tasks & Competencies of Supervision • Assisting the supervisee in development and maintenance of clinical and supervisory records • Interacting with the supervisee in planning, executing, and analyzing supervisory conferences • Assisting the supervisee in evaluation of clinical performance • Assisting the supervisee in developing verbal reporting, writing and editing skills • Sharing information regarding ethical, legal, regulatory and reimbursement aspects of practice • Modeling and facilitating professional conduct • Demonstrating research skills in the clinical or supervisory processes Preparation for Clinical Supervision • Specific curricular offerings from graduate programs • Continuing educational experiences • Research-directed activities that provide insight into the supervisory process • Web resources for clinical supervision support and education – http://www.asha.org/docs/html/PS198500220.html Web Resources • Tips for first time clinical supervisors http://www.asha.org/slp/supervisortips.htm • Special Interest Group 11: Administration & Supervision http://www.asha.org/SLP/SupervisionArticles/ • Frequently asked questions http://www.asha.org/slp/supervisionFAQs.htm • Printed references for clinical supervision http://www.asha.org/academic/teach-tools/phd-prepreferences.htm Continuum of Support Supervisor and Supervisee Process Anderson’s Model (1988) Tool provides a framework for Supervisor and Supervisee to Utilize • Fluid model that supports the individual student’s growth. • The continuum is not time – bound. • Designed to support the supervisee in the development and self-recognition of clinical and professionals strengths as well as the development and self-recognition of those areas requiring additional development of skill. Anderson’s Model (1988) Evaluation-Feedback Stage • Supervisor – Directive in working with supervisee. – Takes “the lead” in planning for the needs of clients with whom the supervisee is serving. • Supervisee – Benefits from specific input and feedback for each client assigned for intervention and/or diagnostic. – Feedback is considered to be ‘direct-active’ in that the supervisee follows supervisor directions. Transitional Stage • Supervisor – Willing to relinquish control. – Provides input and feedback’ however the tone of the relationship becomes more of a joint project. – Use of directive style when necessary. • Supervisee – Begin participating in the planning, implementing and analyzing the course of treatment for clients. – Increased responsibility and planning required for the client. – Increase independence. – Increase client management skills. Self-Supervision Stage • Supervisor – Serves in a collaborative role. – Listens and supports in the problem solving process. • Supervisee – Grows in clinical independence – Plan and implement therapy with less direct supervisory input. – Responsible for primary management of the caseload. Resource • ASHA - Clinical Education and the Professions http://www.asha.org/academic/teachtools/supervision.htm Strategies to Promote Learning • Learner centered teaching/learning focus – what the student is learning – how the student is learning – the conditions under which the student is learning – whether the student is retaining and applying the learning – how current learning positions the student for future learning Strategies • Create positive partnerships/learning environment • Provide encouragement, confidence • Engage in reflective practice Strategies • • • • Model best practices Participate in collaborative problem solving Case presentations Assigned/directed reading with discussion & application to clients • Relate classroom knowledge to clinical experiences Strategies • • • • • Share your clinical teaching “style” Provide specific feedback that leads to change Facilitate peer to peer learning Ask questions that promote learning Evaluate your clinical teaching practices Professional Growth and Development: Active Engagement on the Part of the Student From the beginning, keep the end in mind. • It is essential for the student to – Embrace a long term commitment to their own personal and professional development – Specific strategies include: • Self-analysis through taped observation of assessment and/or treatment sessions • Data collection • Observation of others • Peer interaction/discussion/feedback • Asking and answering questions • Independent goal setting • Commitment to evidence based practice Generic Abilities Is it important to discuss with students? • • • • • • • • • • Commitment to learning Interpersonal skills Communication skills Effective use of time and resources Use of constructive feedback Problem solving Professionalism Responsibility Critical thinking Stress management • May et al., 1995 In addition to demonstration of core knowledge and skills, mastery of generic abilities should yield the following student outcomes: • Generalize from one context to another • Integrate information from different sources • Successfully apply knowledge and skills in practice settings • Synthesize information across domains (cognitive, communication, social, motor, etc.) • Interact effectively with clients, families, the community, and other professionals • Whalen, 2001 The Art of Feedback What makes feedback effective? • • • • • • • Descriptive Specific Responsive Directed to modifiable behavior Solicited Well timed Validated Types of Feedback • Written • Verbal • Scheduled / Spontaneous • Live / Recorded Feedback on Writing • Formula writing • Editing • Electronic records • Volume Role of the Supervisee • Responsibility • Reflection Sounds So Simple Let’s Talk • Time for Questions • Scenarios • Thank you for your interest