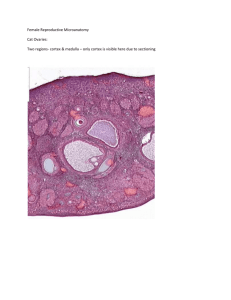
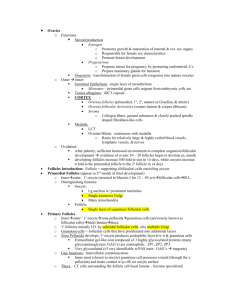
primary follicles
advertisement
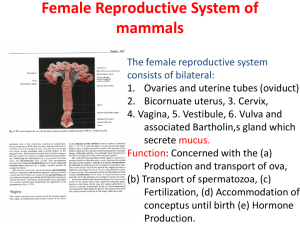
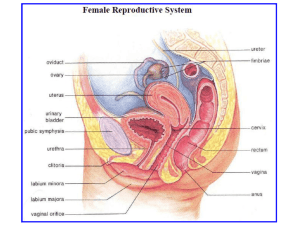
FEMALE REPRODUCTIVE SYSTEM The female reproductive system consists of the internal reproductive organs and the external genitalia • Internal reproductive organs are • External genitalia include -ovaries -oviducts -uterus -vagina -mons pubis -labia majora et minora -clitoris -vestibule of vagina -urethral orifice OVARY Production of gametes and production of steroid hormones are the two major roles of the ovaries, which, therefore have two interrelated functions: gametogenesis (oogenesis) and steroidogenesis Two major groups of steroid hormones are secreted by the ovaries: • Estrogens secreted by ovarian follicles promote growth and maturation of internal and external genitalia • Progesterone secreted by corpus luteum prepare the internal reproductive organs, mainly the uterus, for pregnancy OVARIAN STRUCTURE The ovary is composed of cortex and medulla • Medulla or medullary region – is located in the central portion of the ovary, contains loose connective tissue, blood vessels and nerves • Cortex or cortical region – found in the peripheral portion of the ovary surrounding the medulla, contains the ovarian follicles embedded in a richly cellular connective tissue • The surface of the ovary is covered by tunica albuginea – connective tissue with a single layer of cuboidal cells, called germinal epithelium OVARIAN FOLLICLES Primordial follicles Growing follicles (primary, secondary/ antral follicles) Mature or Graafian follicles • Primordial follicles – are found in the stroma of the cortex just beneath the ovarian surface – a single layer of squamous follicular cells surrounds the oocyte • The primary follicles is the first stage of the growing follicle: follicular cells become cuboidal → between the oocyte and the adjacent follicular cells forming zona pellucida → follicular cells undergo stratification to form the granulosa layer of the primary follicle OVARIAN FOLLICLES • The secondary antral follicle is characterized by a fluidcontaining antrum • Connective tissue investment forms theca folliculi: the theca interna – highly vascularized layer of cudoidal secretory cells; the theca externa – outher layer of connective tissue cells and fibers • The granulosa cells associated with the oocyte form the cumulus oophorus, that project into the antrum. The cells of the cumulus oophorus that immediately surround the oocyte are called corona radiata • The Graafian follicle contains the primary oocyte, surrounded by zona pellucida, corona radiata, follicular fluid, zona granulosa, theca interna and theca externa OVULATION Ovulation is a hormone-mediated process by which the secondary oocyte is released from the Graafian follicle During ovulation the oocyte traverse entire follicular wall including the germinal epithelium due to mechanisms as follows : • Increase in the volume and pressure of the follicular fluid • Enzymatic proteolysis of the follicular wall • Hormonally directed deposition of glycosaminoglycans between the oocyte-cumulus complex and the stratum granulosum • Contraction of the smooth muscle fibers in the theca externa Just before ovulation primary oocyte completes first meiotic division and is transformed into the secondary oocyte, which in its turn is arrested at metaphase of the second meiotic division CORPUS LUTEUM After ovulation the collapsed follicle under the influence of LH undergoes reorganization into corpus luteum This process starts with the formation of the corpus hemorrhagicum with centrally located blood clot Two types of luteal cells are identified: (1) granulosa lutein cells; (2) theca lutein cells Corpus luteum is located within the cortex of the ovary and secretes progesterone The corpus luteum of pregnancy is formed after fertilization and subsequent implantation The corpus luteum of menstruation is formed in the absence of fertilization OVIDUCT (UTERINE, FALLOPIAN TUBE) The oviducts are paired tubes that extend bilaterally from the uterus toward the ovaries The oviducts transmit the ova from the ovary to the uterus and provide the necessary environment for fertilization The wall of the oviduct is composed of three layers: • tunica mucosa – lined by simple columnar epithelium composed of two kinds of cells: (1) ciliated cells; (2) nonciliated, peg cells • tunica muscularis – including inner circular and outer longitudinal layers • tunica serosa – covering mesothelium and a thin layer of submesothelial connective tissue UTERUS All subsequent embryonic and fetal development occurs within the uterus The uterine wall is composed of three layers: • Endometrium, tunica mucosa of the uterus, consists of two layers that differ in structure and function: - stratum functionale – proliferates and degenerates during the menstrual cycle - stratum basale – serves as the source for the regeneration of stratum functionale; lamina propria house the uterine glands • Myometrium – the thickest layer of the uterine wall, composed of three idnistinctly defined layers of smooth muscle • Perimetrium – visceral peritoneal covering of the uterus MENSTRUAL CYCLE Menstrual cycle is controlled, ultimately, by gonadotropins secreted by the pars distalis of the pituitary gland that regulate the steroid secretion of the ovary Phases of menstrual cycle are the defined cyclic changes of the endometrium: • Menstrual phase (days 1 to 4), commencing as hormone production by the ovary declines with the degeneration of the corpus luteum • Proliferative (Follicular, Preovulatory) phase (days 4-14), occuring concurrently with follicular maturation and influenced by ovarian estrogen secretion • Secretory (Luteal, Postovulatory) phase (days 15 to 28), coinciding with the functional activity of the corpus luteum and primarily influenced by progesterone secretion Placenta • Placenta is an extraembryonic organ, responsible for supplying of embryo and fetus with oxygen, nutrients, hormones, antibodies, removal of toxic by-products of metabolism • Consists of two parts – maternal and fetal • Maternal part of placenta – decidual membrane – is a derivative of endometrial functional layer. It includes: (1) decidua basalis; (2) decidua capsularis; (3) decidua parietalis • Fetal part of placenta – the chorion – develops from trophoblast of the blastocyst, it includes chorionic plate and chorionic villi (there are designated primary, secondary, tertiary villi; anchoring and free villi) Placenta: chorion and decidua formation Placental barrier Structures, located in between maternal and fetal blood, which prevent their mixing, are designated as placental barrier. It include • Endothelium of intravillous capillary bed • Intravillous mesenchime • Basement membrane • Cytotrophoblast layer • Syncytiotrophoblast Inactive and lactating breast Light micrograph of the human breast EM of acinar cell from a lactating breast