Recurrence of LCAT deficiency in renal graft (PPT / 5720.5 KB)
advertisement
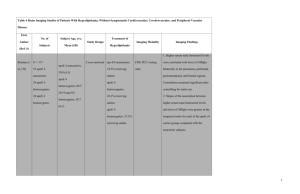
Native and transplant kidney pathology Case 8 Erik Heyerdahl Strøm Dept. of Pathology Oslo University Hospital Rikshospitalet Oslo, Norway ECP Helsinki 30 August 2011 Clinical history Caucasian male 22 years. • • • • • mild edema of lower extremities hematuria proteinuria, increasing to nephrotic level moderate hypertension slightly reduced renal function Suspicion of chronic glomerulonephritis Kidney biopsy was performed PAS Silver staining Silver staining Biopsy diagnosis Glomerular lipid-containing deposits suggestive of Lecithin:cholesterol acyltransferase (LCAT) deficiency Clinical follow-up • Lipid metabolism: – Very low HDL, low LDL, elevated cholesterol and triglycerides • Corneal opacities Genetic testing Compound heterozygous: Two mutations (R244H and M252K) in exon 6 of the LCAT-gene, located on chromosome 16. Final diagnosis: Familial LCAT-deficiency Familial LCAT deficiency Familial LCAT deficiency • autosomal recessive disease • due to a defect in esterification of plasma cholesterol – severe reduction of HDL – elevation of free cholesterol, triglycerides and phospholipids Familial LCAT deficiency lipid-containing depositions within several organs: • kidney – proteinuria, renal failure • cornea – decreased vision • erythrocytes – anemia due to defect of cytoplasmic membrane • aorta and muscular arteries – premature atherosclerotic vascular disease? Familial LCAT deficiency Genetics >70 different mutations described Familial LCAT deficiency Milder disease (”Fish-eye disease”) Kluivenhoven JA: J Lipid Res 2004 ”Fish eye” Corneal opacities: * multiple small greyish spots “foggy” discoloration; band-like at the periphery * impaired vision * present from early childhood in LCAT deficiency Cornea in LCAT disease Cornea in LCAT disease Pathogenesis of renal lesion • Heterogeneous lesions may be due to several mechanisms of disease – deposition of different types of lipid containing molecules, incl. abnormal lipoproteins: Lipoprotein X (Lp-X) – capillary wall impairment – complement activation? Differential diagnosis • renal lesions in chronic liver diseases – ”hepatic glomerulosclerosis” (Sagaguchi H 1965) – Alagilles’s syndrome (hypoplasia of intrahepatic bile ducts) • other lipidoses Case history • Transplanted at 28 yrs, 6 yrs after initial diagnosis • Received kidney from his father, who was heterozygous for LCAT mutation Two days after transplantation Biopsy proven acute rejection Banff IA Biopsy two days after transplantation Protocol biopsy 6 weeks after transplantation Protocol biopsy one year after transplantation CD 68 Recurrence of LCAT deficiency in renal graft • Documented in graft - 7 weeks after transplantation - more than 5 years graft survival What is the significance of the changes in the 2 days post transplant biopsy? 1) Unspecific changes? - probably not 2) Donor derived changes? - probably not 3) Recurrence of disease? - most likely Why present this case? Ultrastructural morphology is quite suggestive of LCAT-deficiency Early recurrence in transplant Coworkers: Dr. Ståle Sund, Dept. of Pathology, Førde Central Hospital, Norway Dr. Morten Reier-Nilsen, Dept. of Medicine, Drammen Hospital, Norway Dr. Christina Dørje, Dept. of Nephrology, Oslo University Hospital, Norway Dr. Trond P. Leren, Dept. of Medical Genetics, Oslo University Hospital, Norway Ultrastruct Pathol 2011:35: 139–45
![Anti-LCAT antibody [EPR1384Y] ab51060 Product datasheet 1 References 3 Images](http://s2.studylib.net/store/data/012077813_1-14f23ab1e19160582ed2e40a91535901-300x300.png)