ppt
advertisement
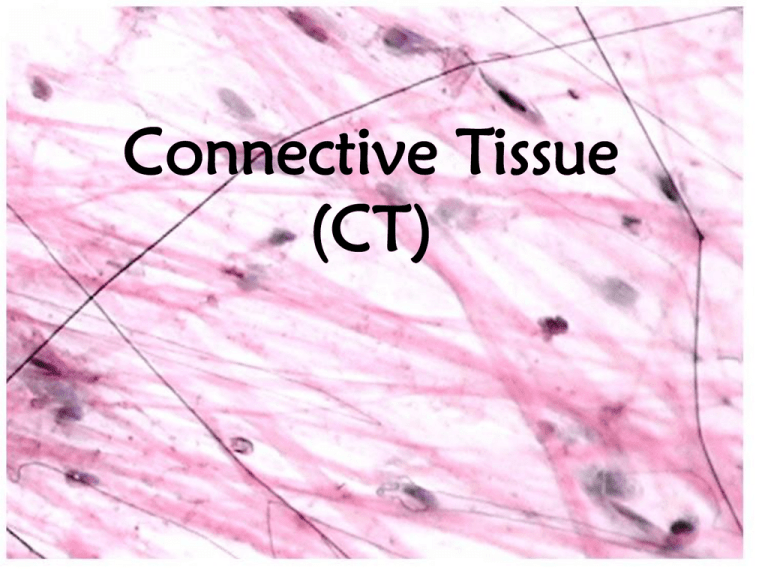
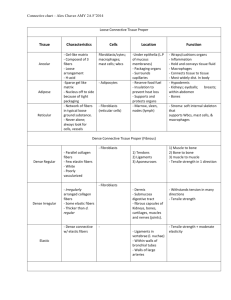
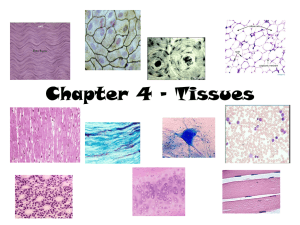
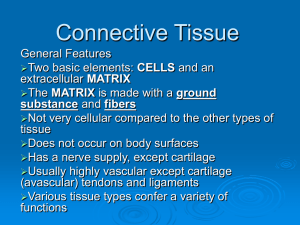
Connective Tissue (CT) Diversity of Connective Tissue Types and Functions: • Loose Connective Tissue: Areolar and fat – insulation, protection (padding), loosely connecting structures • Dense Connective Tissue: Ligaments and tendons – binding and support • Cartilage – protection, support • Bone – support • Blood – transportation Common Characteristics of all CT 3. Composed of different types of cells within 5. All support epithelium 1. Embryonic origin: (mesenchyme) theVariation tissue. in amount of blood supply 4. (vascularization) 2. Has an extracellular matrix of fibers and ground substance. Ground substance Loose Connective Tissue Ex. 1: Areolar – most widely distributed type. – Gelatinous – Loosely packed; lots of liquid held in ground substance – “packing material” cushioning organs, subcutaneous, attaches skin to muscle. – Has all three fibers – Cells: fibroblasts, macrophages, mast cells, and white blood cells – Swells during inflammation (edema) Areolar (Prototype) collagen Ground substance Mast cell Elastin Fibroblast Loose Connective Tissue • Ex. 2: Adipose = Fat! – Loosely packed with sparse matrix – 90% of tissue is mature adipocyte cell – Most of each cell is a fat droplet, so nuclei is displaced to the side – Richly vascularized – Nutrient storage, cushioning in areas like abs, hips, around kidneys – High concentrations subcutaneous (under skin) – shock absorber, insulation – Fat deposits act as local nutrient sources around active organs (heart, muscles) Adipose Adipose Loose Connective Tissue • Ex. 3 Reticular – Only contains reticular fibers. – VERY DELICATE – a fine net of fibers that act as a “soft” skeleton – Supports lympho nodes, bone marrow, spleen, free blood cells. Dense Connective Tissue • Ex. 1: Dense Regular – Tendons and Ligaments – Fibers predominate. – Abundant and crowded fibroblasts make fibers – Little ground substance – Regular, parallel bundles of collagen fibers – Resist tension: pull and stretching. – Ligaments connect bone to bone – Tendons connect muscle to bone. – Poorly vascularized Regularly aligned collagen Fibroblast nuclei Dense Connective Tissue • Ex. 2: Dense Irregular – Thicker, irregularly arranged collagen. – Found where tension is applied in different directions – Example: Dermis of skin, organs, joints Dense Regular Dense Irregular Cartilage Characteristics – Resists tension AND compression – Lots of collagen (strong) AND elastic fibers (flexible) – No nerves or blood vessels – High content of proteoglycans 80% water – Chondroblasts make matrix until end of human adolescence – Mature Chondrocytes found in cavities called lacunae (pit) Hyaline Cartilage • Looks glassy (hyalin = glass) • Few chondrocytes, all found in lacunae • Mostly matrix – lots of collagen • Reduces friction, absorbs pressure • Covers ends of long bones, connects ribs to sternum, forms rings in trachea and bronchi Elastic Cartilage • Looks almost identical to hyaline BUT more elastic fibers more flexible! • Matrix appears more fibrous • More lacunae, closely spaced. • Found in ear and epiglottis Hyaline Cartilage Elastic Cartilage Fibrocartilage • Intermediate between dense regular CT and hyaline • Consists of rows of chondrocytes and collagen fibers • Compressible AND resists tension • Found in intervertebral discs. Bone (Osseous Tissue) • Most supportive tissue in body. • Matrix is similar to cartilage, but with morer collagen (strong) surrounded by calcium salts • Osteoblasts make collagen fibers and calcium salts deposited between fibers. • Well vascularized • Osteocytes stored in lacunae • Bone marrow stores fat and makes blood cells. Blood • Atypical connective tissue • Only classified as such because it arises from same embryonic tissue • Blood cells are within a matrix of blood plasma. • Fibers apparent only when blood clots. How do damaged tissues repair? Injured cells release hormones and proteins to signal need for healthy cells to divide and migrate. Steps to Tissue Repair 1) Regeneration 2) 3) Restore Inflammation Bloodor Supply below scab • Fibrosis Inflammatory Granulation tissue chemicals • • • • released clot, by injured digested by a)replaces Regeneration: cells, macrophages macrophages, replacement w/ same mast cells New capillaries tissue type form. dilate, allowing Fibroblast inreplacement granulation b)Vessels Fibrosis: clotting andcollagen plasma tissue and w/ make fibrous connective proteins and growth tissuefactors. (scar)wbc to invade injured site. Clotting proteins begin clotting. Fibrosis replaces tissue in nonregenerative tissues Regeneration Capacity •Mostly collagen •STRONG but lacks Varies by tissues flexibility/elasticity •Cannot perform function of tissue that was replaced High capacity •Epithelial •Bone •Areolar CT •Dense I. CT •Blood forming tissue •Dense R. CT •Cartilage No capacity •Cardiac Muscle •Nervous Tissue Extracellular Matrix • Embeds cells of connective tissue • Medium for nutrients and other dissolved substances that nourish cells • Made up of ground substance and fibers. • Ground substance – Texture varies •Can be liquid, gel-like, semi-solid or hard. •depends on amount of cell adhesion proteins that trap water called proteoglycans – More proteins, more solid ground substance. • Fibers provide strength and/or flexibility – Allows for weight bearing, withstanding of mechanical abuse, tension – protects!! Dense connective tissue, lots of fibers, little open space. Loose connective tissue: Lots of ground substance – fewer fibers Fibers • Embedded in ground substance • Adds strength/flexibility. • Created by undifferentiated “blast” cells of extracellular matrix • 3 Kinds 1. Collagen: Strong 2. Elastic: Flexible 3. Reticular: Delicate Collagen (white fibers) • Rope-like bundles • Tough, stronger then steel! • Tension resistant Return to fibers Elastic (yellow fibers) • Long, thin • Branching networks • Stretch and recoil ability for elasticity • Highly concentrated in areas like skin, lungs, vessels where elasticity is needed Back to common characteristics of CT Reticular “network” fibers • Short, fine, delicate • Collagenous, but with more give due to branching network • Support soft tissue organs, blood vessels • abundant in boundaries where connective tissue lines other tissues (ex. basement membrane) Blood vessel Collagen Reticular fibers Cells in Matrix • Cells of CT make and maintain the ground substance and fibers of extracellular matrix (ECM). • Each type of CT have immature and mature forms of these cells. • Immature cells have suffix “-blast” – are actively mitotic and produce ECM. – – – – Fibroblasts – make loose and dense CT proper Chondroblasts – make cartilage Osteoblasts – make bone Hematopoeitic stem cells – make blood • Mature cells have suffix “-cyte” – maintain health of matrix – Ex. Fibrocyte • Mature “cyte” cells can reverting to “blasts” to regenerate matrix after injury. What other cells are in CT? • Accessory Cells: – White blood cells (macrophages, plasma cells)– responsible for immune response – Mast cells – responsible for inflammation following injury or infection. – Fat cells – store nutrients Back to common characteristics of CT