PowerPoint Presentation - Slide 1
advertisement

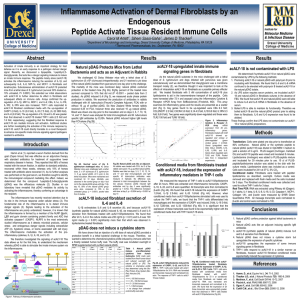
pDAG Stimulates the Inflammasome while Truncated pDAG Downregulates Inflammasome Signaling Alicia M. Holmgren1, Sihem Sassi-Gaha1, James D. Thacker2, Carol M. Artlett1 1Department Abstract The inflammatory peptide, 1-peptidyl-2,3-diacylglyceride (pDAG ) isolated from goat serum, was found to be more effective at curing horses with respiratory disease than antibiotic therapy alone. Previous experiments demonstrated that pDAG was capable of stimulating the production and secretion of proinflammatory cytokines including IL-6, IL-8, and MCP-1 in macrophage. We examined the ability of pDAG peptide to stimulate fibroblasts. Caspase-1, IL-1beta, IL-33, IL-6, IL-8, MCP-1, and MIP-1alpha increased in a dose-dependent manner in normal fibroblasts incubated with pDAG. Furthermore, we found that caspase-1, IL-1 beta, IL-33, IL-6, and MCP-1 increased in a time dependent manner. Further analysis of the signaling of pDAG suggested that it operates through the inflammasome and implies that pDAG is working as a stimulant of the innate immune response. We also analyzed a truncated form of pDAG, which differed from pDAG peptide by the deletion of an isoleucine at the C-terminus. Normal fibroblasts treated with truncated peptide decreased proinflammatory cytokine mRNA levels when compared to controls. To investigate the truncated peptide response further, we analyzed fibroblasts isolated from SSc patients that have elevated inflammasome signaling. The truncated peptide reduced the mRNA transcript levels of many proinflammatory cytokines, such as caspase-1, MCP-1 and IL-33; suggesting that it inhibited inflammasome signaling. This data allows us for the first time to (1) understand the mechanism whereby pDAG is able to stimulate an innate immune response via inflammasome signaling and (2) identify a truncated form of the peptide that reduces aberrant inflammasome activation in a fibrotic disease like SSc. of Microbiology and Immunology, Drexel University College of Medicine, Philadelphia, PA 19129 2TherimuneX Pharmaceuticals, Inc., Doylestown, PA Results pDAG Increases Proinflammatory Cytokines in Normal Fibroblasts Tissue Culture: Normal fibroblasts from a 16 year old individual (GM06112, passage 15), from a 31 year old (GM00024, passage 10 and 12), and fibroblasts from SSc affected lesions, passage 8, were cultured in growth media (Dulbecco’s Modified Eagle’s Medium supplemented with 10% FBS and 1% penicillin/streptomycin) at 37°C and 5% CO2. Transfection: Cells were plated in 500uL of culture medium one day prior to transfection at 50-80% confluence in a 24 well plate. pDAG, truncated pDAG peptide, or no peptide (control) was diluted in Opti-MEM I medium to yield a solution of 5 ug/mL. PLUS reagent (Invitrogen) and pDAG were mixed and incubated 5 minutes. Lipofectamine (Invitrogen) was added to PLUS-pDAG mixture and incubated for 30 minutes prior to use. 0.1 uL-10 uL of pDAG/PLUS/lipofectamine solution was added to a well with 500uL growth media. Incubate 1-3 days at 37°C and 5% CO2. Real Time PCR: RNA was extracted using RNeasy kit (Qiagen). IL-1 alpha, IL-1 beta, IL-6, IL-8, IL-18, IL-33, Caspase-1, MCP-1, Collagen 1A1, and β-actin were measured by SYBR Green Quantitative PCR. All message transcripts were normalized to βactin and control was set to 100. . Conclusions Figure 2: Fibroblasts stimulated with pDAG increase some proinflammatory cytokines in a time-dependent manner. RT-PCR results are normalized to beta-actin and controls are set to 100. Most cytokines are expressed highest after 3 day incubation with pDAG peptide. IL-18 appears to peak earlier, around Day 2. Introduction Hamm et al. (1), reported a serum fraction derived from goat (Capra hircus) that was effective as an adjunctive therapy with standard antibiotics for the treatment of suppurative lower respiratory disease in horses. TherimuneX Pharmaceuticals, Inc. isolated and identified the immunomodulatory compound in the goat serum fraction as 1-peptidyl-2,3-diacylglyceride (pDAG). Initial studies with pDAG have indicated that it triggers the release of proinflammatory cytokines in monocytes and monocyte derived macrophage, such as MCP-1, MIP-1, IL-6, IL-8, and IL-1. Fibroblasts are sentinel cells in skin structures. We therefore extended our studies to normal dermal fibroblasts and investigated the potential for pDAG stimulation of nonimmune cells. The inflammasome is a newly identified inflammatory signaling pathway that triggers the activation and release of the IL-1 family of cytokines (IL-1, IL-18, and IL-33), important mediators of inflammation and the innate immune response. Recent studies from our lab have indicated that the inflammasome is activated in Systemic Sclerosis (SSc). SSc is a fibrotic, TGF-beta driven autoimmune disease, characterized by uncontrolled fibrosis of the dermis and internal organs. During production of a synthetic pDAG peptide a truncated pDAG peptide was developed and tested for immunomodulatory activity. The truncated pDAG peptide was found to down regulate inflammasome activation in SSc fibroblasts. Methods Proinflammatory cytokines, IL-1α & β, IL-33, MCP-1, etc., were increased in a time dependent manner upon fibroblast stimulation with pDAG indicating stimulation of the inflammasome. Truncated pDAG was not able to stimulate proinflammatory cytokine production and even decreased Caspase-1 and Collagen 1A1 mRNA. Truncated pDAG reduced mRNA levels of inflammasome related cytokine below control in SSc fibroblasts. Future Studies Truncated pDAG Does Not Trigger Proinflammatory Cytokines in Normal Fibroblasts Truncated pDAG Decreases Proinflammatory Cytokines in SSc Fibroblasts Determine if pDAG activates the inflammasome using knock-out mice (NALP3-/-, ASC-/-, MyD88-/-, and TRIF-/-). Investigate the cytokine and chemokine profile in mice treated with pDAG by Real Time PCR, immunofluorescence of skin and lung, ELISA of serum, lung, and skin. Flow Cytometry of skin cells for activation: fibroblasts, keratinocytes, macrophages, DCs, mast cells, B cells, and T cells. Western blot analysis of inflammasome components Caspase-1 and NALP3. including Continue work with SSc fibroblasts and truncated pDAG by western blots for inflammasome proteins and ELISA for secreted proinflammatory cytokines and chemokines. Identify the mechanism by which the truncated pDAG decreases collagen production and expression of proinflammatory cytokines and chemokines. References Figure 3: Truncated pDAG is unable to stimulate normal fibroblasts. RT-PCR results are normalized to beta-actin and controls set to 100. Very high concentrations are needed to increase cytokine production using truncated pDAG when compared to pDAG peptide. Collagen 1A1 and caspase-1 expression are dramatically decreased in response to truncated pDAG. Figure 1: Pathway of inflammasome activation. Figure 4: Truncated pDAG decreases proinflammatory cytokines in SSc fibroblasts. RT-PCR results are normalized to beta-actin and controls are set to 100. Fibroblasts were derived from the fibrotic lesions of SSc patients. 1. Hamm, D., et al. 2002. Equine Vet. J. 34(1): 71-5. 2. Kummer, J.A., et al. 2007. J. Histochem. Cytochem. 55(5): 443-52. 3. Martinon, F. 2009. J Leukoc. Biol. 83(3): 507-11.