Respiratory Control
advertisement
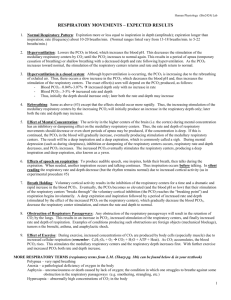
Respiratory Control Voluntary vs Involuntary Control Pathways • Voluntary control pathways pass from motor cortex to lower motor neurons – this pathway bypasses the brainstem centers. • Involuntary control centers are located in the pons-medulla • Spinal or brainstem damage can abolish the involuntary pathway without damaging the voluntary pathway – creating a condition called Ondine’s Curse The Respiratory Rhythm • Respiratory centers in pons-medulla generate a basic respiratory rhythm of bursts of APs • TV is determined by the number of motor neurons active and their rates of activity • The combination of RR and TV that gives an appropriate Valv is optimized to minimize the total work of respiration – this computation requires feedback from lung-chest wall stretch detectors that course in the vagus nerve and exert a burst-terminating inhibition. • Appropriate Valv is determined by integration of inputs that provide respiratory drive. Central and Peripheral Sources of Respiratory Drive Central: – Central chemoreceptors that respond to arterial Pco2 indirectly – they actually measure the pH of the CSF. This works well because dissolved CO2 readily diffuses across the BB barrier and then redissociates in the poorly buffered CSF, whereas ionized acids and bases do not enter the brain readily. – Reticular activating system and other brain centers, including various sensory inputs. Peripheral sources of respiratory drive • Aortic and carotid bodies that are mainly sensitive to arterial PO2 but also to arterial pH and PCO2. Arterial PCO2 is the main source of respiratory drive under resting conditions at sea level Relative ventilation Arterial PO2 becomes really important only when it falls below a threshold value Inputs from central and peripheral chemoreceptors are synergistic In these three experiments, PO2 is varied while PCO2 is held constant at a high, normal or low value. At the arrow, you can see that decreasing alveolar PO2 by 10 mm Hg hardly changes ventilation, while increasing alveolar PCO2 by 10 mmHg increases ventilation by 4.5X. PO2 Altitude Sickness • At high altitude, both PO2 and PCO2 decrease in proportion to the decrease in Patm • As a result, simultaneous conditions of hypoxia (low arterial PO2) and hypocapnia (low arterial PCO2) exist. This causes the symptoms of acute mountain sickness. • This leads to a conflict between the inputs from the peripheral and central chemoreceptors. In the short term of hours to days, it is not possible for the respiratory centers to increase ventilation sufficient to counteract the deficit of oxygen delivery, because they are being inhibited by the central chemoreceptors. Altitude Adaptation • CNS adaptation results as the choroid plexus, which produces the CSF, adjusts the pH of the CSF to a more acid value. This removes the inhibition of respiration caused by the hypocapnia, and PO2 now becomes the most important source of respiratory drive. • The hypoxia results in increased secretion of 2,3 DPG, which improves O2 unloading by rightshifting the Hb-O2 dissociation curve, but this also further compromises O2 loading. Adaptation to respiratory disease • If the disease results in an alveolar ventilation problem (as in asthma) – Both hypoxia and hypercapnia will result • If the disease results in a loss of pulmonary diffusing capacity (fibrotic lung disease, pulmonary edema or emphysema) – O2 uptake will be affected well before CO2 unloading is, because of the difference in the diffusion coefficients. Hyperventilation will result, with consequent hypocapnia. Over time, adaptation will occur and the patient’s hypoxia will become the primary source of his respiratory drive. Be careful with patients that have adapted to chronic hypocapnia – The patient may well stop breathing if – He is anesthetized – O2-based respiratory drive is weaker than CO2 – based drive. – He is switched from breathing room air to breathing pure O2, - this removes his sole remaining reason to breathe. Erythrocyte synthesis and the hematocrit are affected by hypoxia • Hypoxia stimulates release of erythropoietin (EPO) from various tissues (the kidney is a major source). • Increased synthesis of RBCs increases the hematocrit (polycythemia) and thus the blood oxygen carrying capacity – this is the reason that endurance athletes like to train at high altitude, and also why use of EPO and autologous packed-cell transfusion are issues in competitive endurance sports like cycling and Nordic ski racing. • In some individuals who spend prolonged time at high altitude, the hematocrit can rise so high that RBCs tend to sludge in capillaries – this causes chronic mountain sickness. Death at high altitude • A disproportionate fraction of people who die suddenly while mountain climbing at high altitude turn out to have a patent foramen ovale – a perforation of the atrial septum that normally closes shortly after birth. There is a flap that effects the closure, and this normally fuses to close the FO permanently. In some individuals, the fusion does not occur. The sequence of events leading to death runs as follows: 1. 2. 3. 4. Systemic arterioles dilate (due to low blood oxygen and exercise), so TPR falls. Pulmonary arterioles constrict (low oxygen levels in alveolar gas and pulmonary blood), so pulmonary loop resistance rises. If pulmonary resistance rises above TPR, the flap that normally closes the foramen ovale can be pushed open, creating a left-to-right shunt. The shunt has two drastic effects: Pulmonary hypertension leading to pulmonary edema A drop in effective output of the left heart A thought question • In competitive swimming, ability to travel a long distance underwater in one’s initial dive is advantageous • Swimmers were able to increase breath-holding time by voluntary hyperventilation just before diving – why? • However, some of these swimmers became unconscious underwater (why?) and died, and this practice is no longer recommended.


![Respiratory System Lecture:9 [PPT]](http://s2.studylib.net/store/data/010095677_1-807d395ef4decfdd1b95f3c6166ad4e0-300x300.png)