Highlights of Unit 2 mechanical ventilation
advertisement
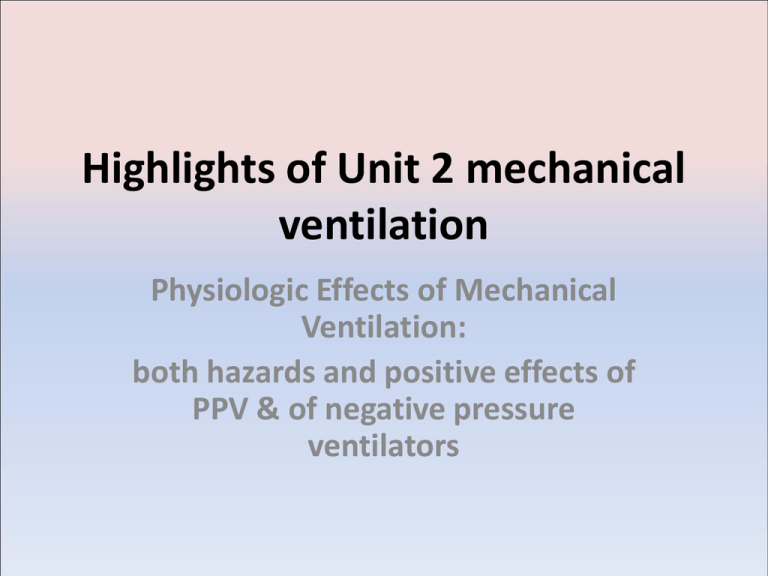
Highlights of Unit 2 mechanical ventilation Physiologic Effects of Mechanical Ventilation: both hazards and positive effects of PPV & of negative pressure ventilators Airway pressures • Spontaneous breathing results in a driving pressure of 0 - -5 = 5 cmH20 • At no point during quiet spontaneous breathing is the intrathoracic pressure positive Airway pressures during PPV • In the case of positive pressure ventilation [PPV], the pressure gradient is positive at the mouth and negative at the alveoli. • The driving pressure is the difference between these two pressures. • the intrapleural pressure will rise because the airway pressure has transmitted through the thin walls of the lung. Cardiovascular effects of PPV • Positive airway pressure raises pressure in thoracic cavity • Prevents the RA from sucking blood back into the heart so the venous return is decreased • Less blood in heart- less blood out of the ventricles so RV and LV both have decreased SV • Compression of pulmonary capillaries • Slows down blood return from head • Decreases Cardiac Output CO • Might decrease the myocardial perfusion Who is more likely to suffer the effects of PPV on cardiovascular system? • The person with hypotension • or with low blood volume Who could benefit from the effects of PPV on the CV system? • patient with congestive heart failure is helpful • need to push back the excess lung fluid • need to decrease the amount of blood returning to the stressed heart, • so that the CO can actually rise with these patients. Effect of PPV on tissue delivery of oxygen • 02 delivery = 02 content (cardiac output) – If decreases the CO ---decrease the delivery of 02 to the tissue – If PPV causes increased VD ventilation, the 02 content can go down Lung Compliance and CO • If the patient’s lungs have normal compliance, 50% of pressure in the lungs is transmitted to the thorax. • • If the patient has stiff, low compliant lung, the higher alveolar pressure may not transmit to the thorax. reverse pulsus paradoxus • status asthmaticus patients placed on PPV can have such excessive driving pressures that this dampens the systemic B/P • decreased LV after load is so low that systemic BP changes significantly between inspiratory phase & expiratory phases. Excessive VT and inappropriately high baseline pressures • Excessive VT and inappropriately high baseline pressures [PEEP] will result in serious problems with CO and with myocardial perfusion. Effects of PPV on hypoxemia • alveolar recruitment, increases surface area for gas exchange so Pa02 rises • as the alveolar C02 drops due to increased movement of gas into the lungs and collapsed alveoli re-inflate the PA02 rises. PPV and hypoxemia with CHF • As we increase the alveolar pressure with PEEP or CPAP, fluid is pushed back and Pa02 rises as more gas diffuses into the capillaries. • As Pa02 rises, the Fi02 can be dropped to avoid 02 toxicity Treatment of hypercapnea with PPV VE rising decreases the PaC02. • VT based on disease states: • 8-10 ml/Kg IBW normal lungs • 6-8 ml/kg IBW asthma • 5-8 ml/ kg IBW for ARDS & for COPD • Keep Pplateau less than 30 cmH20. PPV can increase V/Q • Gas distribution to Zone I instead of Zone III • Pressure on pulmonary capillaries will decrease Q in some areas and raise perfusion to under-inflated areas • Increased Ventilation without perfusion results in increased VD—so PPV can increase VD/VT PPV and acid pH • If VE is too low, respiratory acidosis will result in increased Ventilatory demand • Prolonged acidosis raises the serum potassium so hyperkalemia can cause cardiac arrhythmias PPV and alkalosis • If VE too high: • Prolonged alkalosis will drop the serum potassium so that hypokalemia results- this can also effect the EKG • Alters the Hb/02 affinity with shift to the left so that tissue oxygenation can be decreased • High pH will drop the ventilatory drive and prolong weaning from mechanical ventilation Time constants • Time constant = RAW x C • we need at least 7 time constants for both I & E. PPV and excessive airway pressures • PIP above 50 is associated with lung tissue trauma • If increased RAW, check BBS for suctioning or need for bronchodilator • Pplateau above 30-35 will cause sheer damage. Keep below 30, by decreasing the VT [usually too high for disease] Mean airway pressures • Increasing the PEEP will raise the mPAW • Increasing the Ti will also raise the mPAW • Increased airway pressures raise the FRC which can increase lung C and increase Pa02 but excessive FRC will only add to air trapping Effects of PEEP • PEEP can drop the Cardiac Output particularly in persons with good compliance • PEEP can raise the FRC which may or may not have good effects – Low FRC associated with atelectasis –good – High FRC associated with asthma or COPD- bad • Auto-PEEP created by prolonged Ti can result in air trapping and barotrauma volutrauma. • Excessive VT -- in the face of problems with gas distribution Effect of PPV on VT • If the patient’s parameters are based on pressure, the delivered VT will vary based on the patient’s compliance and RAW. • If ventilation is based on a volume, the airway pressures will vary based due to changes in the patient’s compliance and RAW Effect of PPV on WOB • If WOB is not decreased, settings are wrong – WOB decreased because driving pressure is increased by ventilator – Increased VE drops the PaC02 so ventilatory drive drops – VD/VT decreased because VT is increased – Pa02 rises – If sensitivity set appropriately, there is little WOB Inappropriate settings result in increased WOB • • • • • inspiratory flow rate too low, sensitivity not responsive to patient effort failure to correct hypoxemia failure to correct hypercapnia or acidosis. if the level of auto-PEEP is interfering with triggering a breath Effect on ventilator muscles • muscle atrophy within 72 hours in adults. • muscle mass and muscle fibers affected • resting muscle length increases [due to increased FRC] results in decreased muscle strength, • while alterations in the blood flow to the ventilatory muscles secondary to PPV just adds to the problem. Ventilatory-associated pneumonia [VAP] • VAP more an issue of artificial airways rather than ventilation – cuff pressures to prevent aspiration – oral care Q2 hours, – oral intubation – keeping the HOB Effects on the kidneys • When CO drops, the body shunts blood away from kidney so renal perfusion decreases • Decreased perfusion decreased urine out put – less than 400 ml/day or 160ml/8 hours shift serious – increases in BUN, creatinine , Potassium and decreases in Na. – drug clearance may be affected Serum inappropriate Anti-diuretic hormone [SIADH] • baroreceptors located in the walls of the Aortic Arch and in the carotid arteries respond to decreases of LV pressures by sending a message that results in secretion of ADH so urine output decreases Effects of negative pressure ventilation on the body Major differences • Negative airway pressures more nature, but also negative pressure on the outside of the thorax and on the abdominal cavity • Immobility inside the device– always supine • Not effective ventilation in the face of excessive secretions or other causes of increased RAW • None-invasive so unable to protect airway Negative pressure ventilation • Pooling of venous blood in the abdomen can result in decreased CO • If patient has paralysis, this can result in positional hypotension • If person with Guilliam Barre or myotonic dystrophy may have increased cardiovascular instability– hard to get to patient for CPR • Must decrease VE during nursing procedures Problems with negative pressure ventilation • Chest wall can-- over decades-- become deformed • chest cuirass cover only the chest and not the abdomen so that there is less pooling of venous blood—but maybe less ventilation





![[09]. Strategies for Growth and Managing the Implications of Growth](http://s2.studylib.net/store/data/005486524_1-1f063ac78a31ad020721eab31440cecf-300x300.png)