Nursing Management of the Potential Organ and
advertisement
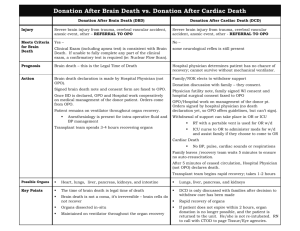
Nursing Management of the Potential Organ and Tissue Donor Susan Ulit, RN, BS, MSN, CNRN Clinical Nurse Specialist Dina Elias, RN,BSN,CCRN Clinical Nurse Educator Objectives • Understand the role of the critical care nurse in the referral of potential organ donor patients • Recognize the importance of the critical care nurse in partnering with OPO representatives • Describe in brief the pathophysiology of brain death and the management goals for the organ donor patient • Understand the role of the critical care nurse as a patient and family advocate during the transition phase of organ donation • Understand the importance of collaboration of healthcare team members in referral and conversion rates and outcomes Referring the Potential Donor • Identify the potential donor in your unit • Be familiar with the hospital’s criteria for clinical triggers • Refer the potential donor to the OPO promptly • Understand the great influence the CCRN has on the process Clinical Triggers Partnering with your OPO • Introduce self to the OPO coordinator assigned to the referral • Encourage collaboration with the OPO member, as they are now an integral member of the health care team • LCSW, Pastoral care, physicians, nursing team • Ask your OPO member to share information and resources • T-4 • Articles in support of donor management Educate Yourself / Team • Policy and Procedures • Become knowledgeable about the different types of donation • Donation after Cardiac Death vs. Brain Death • Become well-informed about organ donation and the pathophysiological effects of brain death • Patient management goals • Realizing the positive impact organ donation brings to all those involved – the “U-turn” Pathophysiology of Brain Death • • • • • • • • • • • Elevated ICP Profound catecholamine response Sustaining CPP Increases afterload LV ischemia/ Myocardial necrosis Decreased LVF Pathophysiology of Brain Death • Herniation of the brain stem • • Ischemia (sympathetic denervation) • • Profound vasodilation • Brain Death = cardiac function + vasodilation Management goals What are the goals? •Organ Perfusion •Organ Oxygenation When does it start? Immediately! Management Goals • Obtain accurate height and weight if not already done (admission) • Line em up!! • Temperature measurement • No tympanic temps (will be inaccurate) • Initial Labs: • CMP • CBC • UA • Coags • Type and cross Management Goals • Timely hemodynamic management • Cornerstone of successful donor management • Management includes: • Ensuring adequate intravascular volume • Maintaining appropriate CO with possible use of vasoactive drips • Initiating T-4 protocol as appropriate • Early recognition and treatment of DI, SIADH, HHNS • Tight glycemic control • Coagulopathy correction Management Goals • • • • • • • • • • • • SBP 90-110 mmHg U/O 1-3 cc/kg HR 60-140 PAWP 7-12 mmHg Serum electrolytes WNL CBC and coags WNL SPO2 >95% PaO2 90-110 pH 7.35-7.5 PCO2 25-45 PF ratio >300 NORMAL PARAMETERS!! Making The “U-Turn” • When a patient dies, despite best efforts, organ donation becomes a positive outcome to a tragic situation. • Hope for Recovery… can become… Hope Through Donation Patient and Family Advocate • Gate keeper • Honor your patients’ and families’ wishes • Uphold a family’s right to be offered the opportunity of organ donation • Do not take that opportunity away by making that decision for them • All health care team members • Leave your personal opinions to yourself Patient and Family Advocate • Promote compassionate communication • Promote collaboration • Be the bridge that links the health care team to patients and their families • Avoid conflict of interest • DO NOT mention organ donation • What is the message we are sending? • What if the family asks about donation? Transition • Brain Death pronouncement • Communicate early and often with the family • Facilitate communication between physicians and the family • Re-iterate prognosis given by physician to ensure understanding • Second Brain Death note is official TOD Team Huddle •Team huddle occurs before discussion of pronouncement with family •Team huddle members include: • • • • • OneLegacy Physician Bedside RN LCSW’s Pastoral Care Transition •Brain death discussion •Patient is DEAD (don’t equivocate) •Transition & decoupling •How to respond to “What’s Next?” •“A specialist will talk with you about the next steps…” •How to introduce OneLegacy •“A member of our healthcare team…” •Donation conversation (OneLegacy) E.O.L. Family Discussion PHASE 1 • MD informs family of grave prognosis DO NOT MENTION DONATION TO FAMILIES “I will get a dedicated family specialist to speak with you” Family must be given time alone to process this new information National HRSA Collaborative Best Practices CMS / Joint Commission Mandate 42. CFR 482.45 HUCLA Policy 316, Data accessed Nov. 24, 2009 PHASE 2 Family is presented with donation options by trained designated requestor only! Collaboration = Higher Consent Rate • Organ donation consent rate highest when hospital staff and OPO approach together Source: “Improving the Request Process to Increase Family Consent for Organ Donation”; Gortmaker, et.al. (Journal of Transplant Coordination 1998; 8:210-217) Summary • Educate! • Advocate! • Collaborate! • What you say and do can make the difference between a yes and a no.