blood lab
advertisement
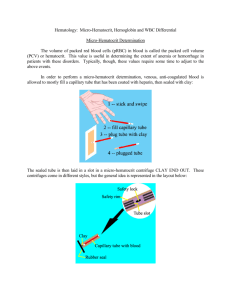
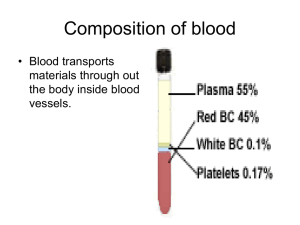
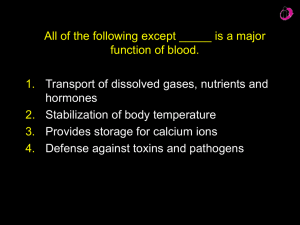
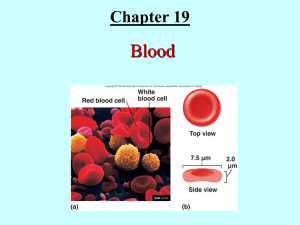
Biology 161 Blood Lab Scott.lehbauer@lethbridgecollege.ab.ca In this Lab 1. 2. 3. 4. 5. Hematocrit Reading Measuring Hemoglobin Blood Differential (White Blood Cells) Identifying Blood Disorders Blood Typing (Examples Only) Hematocrit Defn. - The percentage of total blood volume occupied by erythrocytes. Hematocrit increases with polycythemia and dehydration and decreases with anemia. Polycythemia – an abnormally high number of erythrocytes. Anemia – reduced oxygen carrying ability in the blood due to too few erythrocytes or abnormal hemoglobin. Hematocrit Reading Layers Top The Yellow – plasma collects at the top Middle The Buffer Coat - The White Blood Cells Bottom The Red – RBC’s Collected at the bottom of the hematocrit tube. Normal Hematocrit Readings Males – 40 to 50 % (5,200,000 RBC’s / mm3) Females – 37 to 47% (4,700,000 RBC’s/ mm3) Hemoglobin • The basic way to compare blood by color on the color chart. • Orange indicates anemia. • Deep Red indicates normal hemoglobin. Normal Hemoglobin Readings • Males – 13 to 18 g/100ml • Females - 12 – 16 g/100ml White Blood Cells (Leukocytes) White blood cells are grouped in to two major categories, Granulocytes and Agranulocytes. Granulocytes – are roughly spherical in shape, they are larger than RBC’s, have lobed nuclei, and their cytoplasmic granules stain specific colors with Wright’s Stain. Agranulocytes – are WBC’s that lack visible cytoplasmic granules. Their Nuclei are typically spherical or kidney shaped. WBC’s - Granulocytes Basophils (0-2%) – • release heparin and histamine. • The granules stain purple and the deep purple • lobed nucleus has two or three constrictions. WBC’s - Granulocytes Eosinophils (0-4%) • fight allergies. • They have a bi-lobed nucleus • red cytoplasmic granules. WBC’s - Granulocytes Neutrophils (60-70%) – • 1st WBC to an infection • mature neutrophils have a 4-5 lobed nucleus • cytoplasmic granules stain mauve. WBC’s - Agranulocytes Monocytes (4-9%) – • carry out phagocytosis ie. macrophages. • These are the largest White Blood Cells. • The nucleus is a U-shape • the cytoplasm is a greyblue color. WBC’s - Agranulocytes Lymphocytes (20-25%) • provide immunity: • T and B cells. • These are the smallest WBC’s. • The nucleus of these cells is spherical and takes up most of the cell. Differential Note- when beginning your differential, RBC’s normally cover the entire field of view. Differential – is a comparison by numbers of the numbers and type of white blood cells on a person’s blood slide. This is used to determine if there is a diagnostic increase of a certain type of cells. To do a differential we will sequentially go back a forth across the blood slide, count 50 WBC’s and double the number to give us a percentage. Blood Typing • Transfusion of the wrong blood type into an individual can be fatal • Red Blood Cell Plasma membranes have highly specific glycoproteins at their external surfaces called “antigens” • Presence or absence of each antigen allows each person’s blood cells to be classified into blood groups Blood Typing Antigen – • from the words antibody generating is a molecule that sometimes stimulates an immune response • are highly specific glycoproteins that are at a red blood cells external surface (surface antigens) Agglutinogen – • since the RBC antigens promote agglutination they are called Agglutinogens Blood Typing Antibody – is a protein molecule that is released by a plasma cell that binds to a specific antigen. • are proteins found in the blood that are used by the immune system to identify and neutralize foreign objects Agglutinin – • preformed antibodies that act against RBC’s carrying the ABO antigens • Found in the plasma Agglutination • Involves red blood cells and can be used to identify RBC surface antigens (with known antibodies) or to screen for antibodies (with RBCs with known surface antigens). • When faced with a different blood type the donor’s red blood cells are attacked by the recipients plasma agglutinins • Clumping of the RBC’s occurs ABO Blood Groups • ABO blood groups are based on the presence or absence of two agglutinogens type A or type B • The use of serum containing the plasma antibodies, agglutinins, is used to cause the agglutination of the blood and identify type according to the surface antigens present Blood Types AB – has both A and B surface antigens, and has neither anti-A nor anti-B antibodies in it’s plasma. • Therefore AB blood types can receive blood from any blood type but can only donate to another AB blood type. B – has B surface antigens, and has anti A antibodies in it’s plasma • Therefore B blood types can receive blood from type B or type O and donate blood to type B or type AB Blood Types A – contains A surface antigens and anti – B antibodies in it’s plasma. • Therefore A blood types can receive blood from type A and type O and donate blood to type A and type AB. O – has neither type A or type B surface antigens and has both anti- A and anti- B antibodies in its plasma • Therefore O blood types can receive blood from type O and donate blood to type A, B and AB (Universal donor) Blood Typing Rh Factor • This blood typing system was named due to one Rh antigen (agglutinogen D) was first isolated in a Rhesus monkey. It was later found in humans. • About 85% of Americans are Rh+ • As a rule a person’s Rh and ABO blood types are reported together for example A+ or B- or O+ Rh Factor • Anti Rh antibodies are not spontaneously formed in the blood. • However if a Rh- person receives Rh+ blood in a transfusion the immune system will produce anti Rh antibodies • After the second transfusion the same agglutination patterns can be seen • Hence the problems that occur with Erythroblastosis fetalis (hemolytic disease of the newborn) Normal Blood Slide Erythroblastosis Fetalis • This may occur when an Rh- mother has her second Rh+ baby. • Bleeding from the placenta detaching from the uterus causes antigens from the Rh+ newborn to pass into the mother’s blood stream. • Without treatment the mother will develop anti Rh antibodies which are then passed to the next Rh+ baby which destroys the newborns red blood cells Erythroblastosis Fetalis • causes hemolysis of immature RBC’s (erythroblasts = reticulocytes) which are nucleated RBC’s. • Note the prickly cells. The baby suffers from anemia because the RBC’s die before they can carry oxygen. Leukemia Leukocytosis (increase in WBC’s but they are immature and incapable of performing immune function) • There is a decrease in the number of RBC’s and thrombocytes so there is anemia and pinpoint bleeding and bruising. Infectious Mononucleosis Commonly called the “kissing disease” this highly contagious viral disease often seen in young adults. • It is caused by the Epstein-Barr virus and is characterized in the blood by an increase in the number of lymphocytes and monocytes (atypical lymphocytes). • 50 – 95% of the WBC’s present may be lymphocytes and monocytes (normal 35%). • The WBC count will also increase from 7,000 to 11,000 per cubic mm to 20,000 WBC / mm3 Sickle Cell Anemia Is caused by the abnormal hemoglobin (HbS) rather than HbA. • The cells become sickle in shape and can’t carry oxygen well causing anemia. • They become stuck together and clog capillaries. • These events interfere with oxygen delivery, and during increased respiration leave the victim in pain and gasping for air. Hypochromic Anemia • Erythrocytes are small and pale. • This is caused either as a secondary response to a hemorrhagic anemia, or from an inadequate intake of iron in the diet. Midterm Exam 1 • February 28th in EC Fredricks Theatre (5pm – 8pm) • 21 questions with A an B parts • 1 minute per slide on power point • Practice exam to be posted this week • Urinalysis cups to be given out at exam, bring full to next lab.