Future of Medical Schemes
advertisement
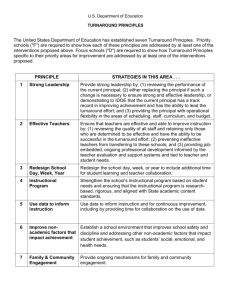
Our Response The Eastern Cape – a compelling place to live, work, play and enjoy wellness South African realities • R79bn on 85% uninsured population • R84bn on 15% insured population (7m population) • The EC has a budget of R14.2bn for 7m population • National revenue will not increase significantly and health’s portion unlikely to grow much • SA has poor health outcomes in terms of equivalent middle income countries • Therefore we have to do more with less and spend prudently Provincial Reality – • • • • Budget Overspend Escalation 2010 budget need 2009 2010 R 11. 8b R 2.4b R 1.4b R 15.6b R 13.6b R 1.6b R 1.5b R 16.6b • Actual Budget R 13.3b R 14.2b • Deficit R 2.3b R 2.4b The population of the EC is +/- 7m and is equal to Medical Scheme population However, their budget = R84b !! Budget 2010/11 • Accruals 2009/10 R 1.4b • Top slice R 444.2m (R1.7b over MTEF for projected overspend) • Conditional grants cut by R 82.9m (R317.8m over MTEF) • Accruals 2010/11 R1.2b + R 400m overdraft • Unfunded OSD & HRopt caused COE to increase from R6.26b to R 7.92b (by R1.6b or 26%) • Unfunded HRopt is R468m + R9m pm • COE increases to 63.6% and G&S to decrease by 8% (actual) or 13% against revised estimates Budget 2010/11 • Total Budget R 14.237b which includes the Priority alloc. R 197.4m (R1.1b over MTEF) • Increase of R394 Million or 2.8% from the 2010/11 adjusted appropriation (R13,842b) • However, decrease of R871 million or 5.8% as against the 2010/11 revised estimate • With Inflation – decrease of 3.7% of approp. & decrease of 11.2% of dept. expenditure estimates. EC Peculiarities: • Unstable and fractured department • Demotivated; disempowered & inappropriate staff • Budget cuts and inappropriate expenditure • 5 different MECs in last 4 years • 4 different HODs in last 4 years • Treasury whose idea of a turn-around strategy is cost- cutting • High vacancy in critical posts with a moratorium on non-clinical posts EC Peculiarities: • Per capita alloc. does not take into account cost of delivery • Poor infrastructure (roads; water & elect) • SDP has 68 dist. hosps; 2 regional hosps and 5 tertiary hosps – too many; dysfunctional; poor condition & poorly managed • R26b infrastructure with R1.2b budget • Admin increase by 159.8% vs. Clinical increase of <2% (inappropriate staff) • Fraud & Corruption Provincial Challenges: 1. Budgeting Process: • Historical vs. Activity vs. Performance (Cluster) vs. Needs / Demographic based budgeting 2. Performance Budgeting: • Merging of financial and non – financial info. • Optimum usage of resources • Enhanced service delivery outputs & inputs • Linking our limited resources to results & outputs • Increase efficiency and effectiveness 3. Organisational Development: • Rationalized SDP with PHC approach Challenges: 4. Financial Management, Environment & HR Mx & Leadership • Repeated poor audits despite numerous interventions • Poor Financial Mx with a lack of competent capacity at many levels resulting in negative audit opinions • The negative audit outcomes will continue until the fundamentals are not addressed - which are the effective facilitation of the Financial Control Environment, Financial Control Activities, Financial Information and Communication, Financial Monitoring and Evaluation Activities • Transversal IT systems with Connectivity Health Sector Plan Do More with less by: – Social Compact to prevent diseases & over utilisation of facilities – Re-engineer Business (RPHC towards NHI -prevention is better than cure) – Improve procurement to get value-for-money – Increase efficiency & effectiveness e.g. decentralise with central M&E and sometimes central co-ordination – Income Generation: (NHI compliant services/ facilities) Social Compact • Responsibility for health – “I am responsible; We are responsible & South Africa is responsible” • Prevention – – – – MVA Mass HCT program Circumcision Substance abuse etc etc • Participation – DHA – Selection of providers for training & serving community • CHP • Nurses • Doctors Procurement Plan • • • • • • Transparency with second bite principle Value-for-money No “Winner takes all” Reserve suppliers Devolved administration with budgets LED Supplier 1 Equipment 1 Supplier 2 Supplier 3 Supplier 4 x equipment 2 x equipment 3 x equipment 4 x equipment 5 equipment 6 x x equipment 7 x equipment 8 equipment 9 equipment 10 equipment 11 Supplier 5 x x x Turn-around Plans: 1. 2. 3. 4. 5. 6. Revenue Generation Clinical Health Services Turnaround Finance Turnaround Integrated Human Resources Mx Turnaround Infrastructure Turnaround & Accommodation plans Information Systems (incl. VPN, Patient Registration System) 7. Monitoring and Evaluation HR Turnaround Plans: • • • • • • • Organogram to address functionality Person to post matching Persal cleanup and document management Electronic leave management Contract employees cleanup Compliance monitoring tool HRD plans – Social compact – Grant Mx – Improve Training capacity Finance Turnaround: • • • • • • • • Re-alignment to meet function Austerity measures & Finance t/o plan Audit interventions SCM revamp & Mx of declarations & delegations Logis implementation Finance Monitoring tool Revenue Generation Fraud Mx Infrastructure Turnaround: • IDIP • IRM update • Preferred SCM process & policy with own BEC and BAC • Re-prioritization of project – RPHC • Maintenance contracts • Health Technology committee • Re-alignment with DHS • IT plans Clinical Turnaround: • • • • • • • • • Revitalization of PHC Priority sub-districts development Quality outcome management HCT & TB campaign PBM Radiology plans EMS plans IT – integrated DHIS Academic platform Health Reform Timeline Revise tax incentives Create risk Equalisation fund Mandate restricted membership schemes Gov. sponsored low-income scheme Medical schemes Act 2003 1998 Mandate public sector coverage 2003 2004 2003 Mandate medical scheme membership 2005 2005 2004 Introduce differentiated amenities Introduce PSCF Set up legislation PSCF authority Create legislation Introduce revised for autonomous hospital public hospitals reimbursement (special system dispensation) Source: Social Security Committee Presentation Introduce mandatory environment Get the Balance Right Costs Equity Efficiency Quality “To provide care of the highest possible quality, at the least possible cost” Prof. Edward Hughes