Mental Illness and Suicidal
Behaviour in Children and Youth
Dr Phil Ritchie, Psychologist
Children’s Hospital of Eastern Ontario
Mental Illness in Children
and Youth
• Statistics suggest that by the time students graduate
from high school, 1 in 5 will have met criteria for a
diagnosable mental illness.
• Unfortunately, only 1 in 6 of these will have received
appropriate treatment for this.
Adolescence
• The period of life when your child kicks you off the
pedestal they’d put you on only to step up onto it
themselves.
• That period that immediately follows your child’s first
sleeping through the night in which they decide to
stay up all night and sleep through the day.
Adolescence – A Series of Crises (with
thanks to Dr. Tracy Vaillancourt)
– Identity – increasingly self-conscious, who do they
want to affiliate with, sexuality
– Autonomy – move away from parental influence to
that of peers
– Intimacy – relationships no longer based on
common activities, now focuses on meeting
emotional needs
A Series of Crises cont’d
– Sexuality – biologically driven
– Risk-taking – stimulation-seeking
– Egocentrism – concerned with how others
perceive them
The Adolescent Brain
• Brain develops to mid-20s
• At puberty, pruning process
• Motor and sensory areas are quite sophisticated
while decision-making (important for impulse-control
and emotional regulation) centres remain
underdeveloped
The Adolescent Brain cont’d
• In short, adolescents are physically capable of
complex feats, but psychologically ill-prepared to
make good decisions
• One giant, tingly nerve looking to get stimulated but
little judgment about the dangers such stimulation
might entail
•
The Adolescent Brain, cont’d
Anxiety Disorders in Youth
– A Pattern of False Alarms
• Anxiety is a good thing – anticipating future danger or
misfortune is helpful
• Keeps us from diving into unknown waters or walking
in a dangerous neighbourhood late at night
• When anxiety becomes extreme or irrational, it goes
from adaptive to maladaptive
• Most common Mental Illness affecting 12% of
population, half of which will develop as children or
youth
Anxiety Disorders in Youth cont’d
•
•
•
•
•
•
•
•
Panic Disorder
Specific Phobia
Social Phobia (Social Anxiety Disorder)
Obsessive Compulsive Disorder)
PTSD (the only 1 that requires a “trigger” event)
Generalized Anxiety Disorder
Separation Anxiety Disorder
Anxiety Disorder NOS
Anxiety Disorders in Youth cont’d
• In general, in order to meet criteria as an anxiety
disorder, the associated fear may be recognized as
excessive or unreasonable (though sometimes,
particularly in children this may not be the case), is
not just a brief and passing phenomenon, and is
interfering with regular development/normal
functioning.
Treating Anxiety Disorders
• Cognitive Behaviour Therapy (CBT) is evidencedbased non-medication treatment of choice
• Mood, thoughts, and actions inextricably linked
• You are their teacher, not therapist, but helpful to
understand principles (e.g., exposure/response
prevention)
Classroom Accommodations for
the Anxious Student
• Check in with student on arrival
• Don’t penalize for being late (sx at home often
interfere with getting out the door)
• Assist with peer interactions
• Anticipate difficulty with transitions
• Give notice re. changes in routine
Classroom Accommodations cont’d
• Extra time for tests and assignments
• Safe place
• Use of nonverbal cues so as not to centre out the
student
• Model appropriate coping behaviours
Interventions for the
Anxious Student
• Worry
– Answer the “what ifs” and take away anxiety
associated with the unknown
– Track improvements with feedback to the student
– Have the student rate their fear and then track it
Interventions for the
Anxious Student cont’d
• Emotional Outbursts
– Identify triggers with the student
– Encourage them to problem-solve (e.g., CPS)
– Develop a hierarchy of safe places in which to deescalate from a meltdown
Mood Disorders in Youth
•
•
•
•
Major Depressive Disorder
Dysthymic Disorder
Bipolar I and II Disorders
Cyclothymic Disorder
Mood Disorders cont’d
• Important to understand that mood disorders affect
not just how the student feels, but also sleep,
appetite, concentration, motivation, interests, and
energy.
• This is a recipe for a decline in functioning at school
(as well as home and social), likely to compound an
already fragile self-esteem.
• Treat depression and other factors tend to improve.
Suicidal Behaviour in Children and Youth
• With thanks to Dr. Allison Kennedy
A Complicated World for
Teens
• Amanda Todd’s video has almost 6 million views,
almost 45 thousand likes, and almost 100 thousand
comments
• There are a number of RIP Amanda Todd Facebook
sites with 100 of thousands of likes
• Adolescents have unprecedented access to unfiltered
information about suicide through social media and
the Internet
Social Media – A Pox on All Our Houses?
• Preliminary studies suggest that internet use in a
country was associate with an increase in suicides.
• Cyberbullying has been tied to increased suicide
risks particularly in adolescents.
• Social media may help people form suicide pacts and
unlike more traditional pacts, may involve complete
strangers and bogus participants/eggers on.
• Internet provides a “how-to” guide for suicide.
• Internet provides access to pro-suicide sites.
Social Media – A Pox on All Our Houses?
• But social media are also being used to prevent
suicide.
• National Suicide Prevention Lifeline (US) developed
a Facebook chat add-on for users to report at-risk
individuals.
• Similar links being developed for Twitter, Tumblr, and
Google (e.g., “I want to kill myself” results in top
sponsored link being to prevention resources)
Canadian trends
• In Canada, suicide is 3rd leading cause of death for
10 to 14-year-olds and the 2nd leading cause for 15 to
19 year olds
• In Canada, suicide is the cause of death for 24% of
16 to 24-year-olds
• A large percentage of youth experience suicidal
thoughts
• At CHEO, youth are increasingly presenting to the
ED with suicidal risk
Reasons for suicidal
behaviour in adolescence
• Changes in cognitive development
– capacity for abstract and complex thinking
– more capable of contemplating life circumstances,
envisioning a hopeless future, suicide as a possible
solution and planning and executing a suicide attempt
• Onset of substance use/abuse
• Increased rates of mental health problems
• Increased access to potentially lethal suicidal means
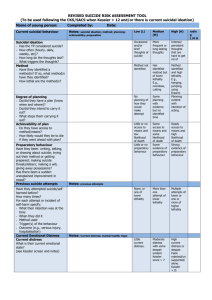
Risk: Clinical factors
• Psychiatric history
– Depression and conduct disorder
• Drug/alcohol use
• Previous suicide attempt
• Hopelessness
Risk: Personal and family
history
• History of abuse
• Family history of suicide/exposure to suicide
– Exposure reduces the suicidal taboo
• Issues with family communication and problem
solving
– Attachment issues, inability to approach parents for support
Risk: Life stressors
• Suicidal adolescents present with significantly
increased levels of life stress
• Increased interpersonal conflict and social isolation
• Other stressors may serve as a trigger to vulnerable
youth who are already at risk (e.g., loss, transition)
Risk: Emotional and
cognitive factors
• Problem solving deficits
– Difficulty generating alternative solutions to interpersonal
conflict
• Poor emotional regulation
• Impulsivity
Sex differences
• Adolescent girls also are more likely than boys to
attempt suicide --- although boys are more likely to
complete it (3 males:1 female)
• Most studies relate the differences in completion
rates to the method chosen
– Girls --- overdose or cutting
– Boys --- hanging or firearms
Other demographic risk
factors
• Age
– Increased risk with increased age within the teen years
• Race
– Aboriginal youth at particularly high risk
• Sexual orientation
– Gay/transgendered youth at higher risk
Some Statistics …
• 15 to 20% seriously consider suicide
• 10 to 15% make a suicidal plan
• 6 to 9% attempt suicide
• 2 to 3% present for necessary medical treatment
after a suicide attempt
… in a classroom
• 4 or 5 students will seriously consider suicide
• 3 students will have a suicidal plan
• 2 students will attempt suicide
• Students in an alternative setting are at higher risk for
suicidal behaviour
How school staff can help
• Learn
– … the signs of risk in students
• Identify
– … at risk students
• Refer
– … to appropriate resources
Warning signs in school
• Suicidal threats
• Talking or writing about death, dying, suicide
• Changes in appearance, mood, attendance,
academic functioning
• Social isolation
• Bullying
Talking to at-risk students
• Know your limits
• Listen
– Acknowledge feelings, clarify, summarize, validate
• Know your resources
• Act and ask: “have you thought about killing yourself;
have you already tried to hurt yourself?”
• Follow up
School based prevention
•
•
•
•
•
Be aware of signs and know how to respond
Foster a healthy school environment
Educate students on coping skills
De-stigmatize mental health issues by talking about it
Educate students regarding mental health resources
in the community
Non Suicidal Self Injury
(NSSI)
• Intentional self-harm without conscious suicidal intent
(e.g., cutting, scratching, burning, hitting)
• Relatively common, particularly for girls
• An attempt to cope that is often learned from other
youth
• Primary goal of behaviour is affect regulation
• Youth who engage in NSSI are at elevated risk for
suicidal behaviour
Assessment of nonsuicidal
self-harm
• Examine onset, frequency, intensity, and duration
• Assess risk of injury
• Identify triggers
The role of parents/caregivers
• Engage parents whenever possible
• Parents need to be aware of safety issues
• Parents need guidance regarding how to respond if their teen
approaches them
– Stay calm, listen, don’t judge, provide comfort and reassurance
(e.g., “I know that you are in a lot of pain right now but I am with
you and we will get you the help you need to feel better”)
– Parents can call crisis lines directly
• Even if the teen does not feel comfortable directly confiding in
them, they can check in, monitor, and assist with distraction
during an episode of acute distress
• In general, parents and professionals provide better support
than peers
Follow-up – the elephant in
the room?
• Having asked “the question” and referred to a school,
community, or hospital-based resource, as
appropriate, it is important to re-establish your
relationship with the student.
• Make time to see the student the next available
opportunity, let the student know how glad you are
that s/he spoke with you, that you care about how
they’re doing, but that you will leave it to the mental
health professionals to deal with that part of things.
• And that if s/he wants to talk again, you’re always
happy to listen, and that this doesn’t otherwise
change anything about the relationship.
The Adult (i.e., Teacher) Brain (with thanks to Dr.
Matthew Sharps)
• When communicating with anyone in crisis, important
to understand how it affects not only their thinking,
but also ours.
• Big stress response (HPA Axis) results in blood being
diverted from neocortex to lower areas (limbic and
reptilian brains)
The Adult Brain cont’d
• Go into survival mode and the reptilian brain kicks in
• Alligators are brilliant survivors, “living fossils” that
have existed 200M years
• Alligators are not so good at conversation,
investment advice, or problem-solving in the midst of
crisis
The Adult Brain cont’d
• In survival mode, we get “alligator stupid”
• Reptilian brain is reliable but rigid and compulsive
• “Four Fs” – feeding, fleeing, freezing, and mating
The Adult Brain cont’d
• Survival mode is a vestige of our hunter/gatherer
brain
• Tunnel vision can be helpful if pursuing a wild boar
looking to turn it into dinner
• Not so helpful if staring at the hickey on our teenage
daughter’s neck or the crack in the new HDTV after
our son invited a “few friends” over c/o Facebook
while we were out of town
The Adult Brain cont’d
• Need our neo-cortex for more advanced problemsolving (don’t try to fit head in peanut butter jar – get
a spoon)
• Also need the neo-cortex to manage sub-cortical
parts of brain, and to separate affect from problemsolving
Alligator Stupid - There is No “Us and Them”
• While negotiating with those in crisis, important to get
out/stay out of “alligator stupid” mode, and have the
higher centres of the brain remain active
• Those with a past of early trauma, chronic stress, bad
night’s sleep, or 12 skinny pumpkin spice lattés (they
were on sale) compound matters
Alligator Wrestling
• When appropriate, taking a few slow, big breaths can
help
• Your paraverbals – calm, not too loud, not too fast,
but reassuring
• Become their surrogate neo-cortex – get them to
slow down, help them see that there are other
solutions
Web-Based Resources
• www.cheo.on.ca
• www.ementalhealth.ca
• http://www.kidsmentalhealth.ca/children_youth/learn_
more.php
• http://www2.massgeneral.org/schoolpsychiatry/for_ed
ucators.asp