Integumentary System
advertisement

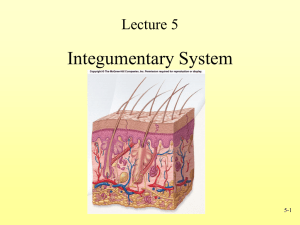
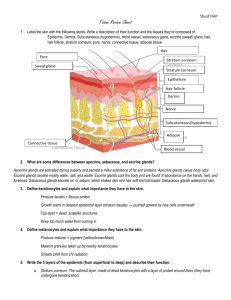
Chapter 4 Guiding Question: What are the components of the integumentary system? Not just a covering for the body • Largest organ Blood vessels, connective tissue structures, glands, hair, nails, nerves, skin • Plays a large role in homeostasis Has inherent and adaptive • Calluses • Darken in sun • Elasticity • Sensitive to moisture characteristics Guiding Questions: 1.) What embryonic layers form the integumentary system? 2.) Describe the development of the integumentary system. 3.) What are some various causes of hair loss? Ectoderm & mesoderm in origin Skin is a complex structure Many things can go wrong in its development Let’s make a timeline! Simple ectoderm epithelium over mesenchyme • outermost layer of skin form a simple squamous tissue that becomes stratified as the embryo develops from the ectoderm Deeper parts of skin begin to form from mesoderm (dermis, hypodermis) 8-9 wks: mesenchyme begins to mature and fibroblasts form, and dents occur in the upper squamous layer form lanugo. • 10 weeks: ridges form between the outer and inner layers of skin—so don’t separate when rubbed • 11 weeks: small nails at the tips of fingers & toes, followed by development of special blood vessels in the layers of skin Angiogenic factors stimulate the production of these vessels • 20 weeks: Glandular structures form Inward growths of the outermost squamous cell layer Will eventually produce oils and sweat • 25 weeks: Pigmentation • About 26 weeks: melanoblasts mature into melanocytes (build pigments) • nervous tissue structures develop What are the three major layers of the skin? Describe the basic characteristics of the three major layers of the skin (recommend a chart) 1. Epidermis: Epithelial Superficial & thinnest cells are very tightly packed New cells produced here 2. Dermis: Connective Deep to epidermis & thick Primarily connective tissue loosely packed cells 3. Subcutaneous/Hypodermis (adipose tissue) • Deep to the skin/dermis • Layer of insulation Outermost: Stratum corneum • Dry, dead, • keratin filled (waterproof, tough) Stratum Granulosum • Waterproof • Contains granules of keratin Stratum Spinosum • “Prickly” layer • Contains Langerhans cells (fight infections) Stratum germinativum / basale • Cells undergoing mitosis, move up and horizontally • Contains malpighian layer or “Pigment layer” with melanosomes • Forms epidermal ridges Stratum corneum: Dead squamous cells Stratum lucidum: (only in thick skin); oils from lysosome disintegration Stratum granulosum: Granules with lipids and keratin – forms waterproof layer Stratum Spinosum: cuboidal cells, desmosomes hold together >> spiny Stratum Germinativum/ Basale: dividing columnar cells Specialized cells within epidermis: • Melanocytes Melanin: pigment, inc. w/sun (protection) • Keratinocytes Keratin: tough, waterproof material Abrasion resistance for cells • Langerhans cells Immune response against microbes invading the skin Second layer of the skin Collagen, elastin fibers– scattered Dense, irregular connective tissue Loose, connective tissue = areolar connective tissue • Binds blood vessels, membranes, muscles, nerves, and skin to other structures • Contains extensive meshwork of protein fibers (fibroblasts) Involved primarily in body growth Connective tissue maintenance Wound healing Dermal papillae: parallel rows of peg-like projections • Unique to each individual; akin to fingerprints Third layer of the skin Third, innermost layer of the skin Thickness, composition vary throughout body Composed of loosely-arranged elastic fibers that anchor the skin to the fascia • Sheet of fibrous connective tissue • Covers muscles, skull bones, some organs Large amount of adipose (fat) cells Large network of blood vessels, capillaries, lymphatic vessels Glands Nerves Nails Hair 3 Types: • Ceruminous • Sebaceous • Sweat/sudoriferous Produce cerumen (waxy secretion), an apocrine secretion (ear wax) Found lining ear canal Holocrine glands (secrete whole dead cells) Produce, store abundance of fat, which burst and die, releasing sebum Sebaceous Glands • Secrete oil (sebum) for hair/skin • Ducts open into hair follicles • Accumulated sebum enlarges ducts>>white heads • Darkened sebum>>black head Sudoriferous/Sweat • Eccrine Glands Widespread Watery Fluid Separate pore • Apocrine Glands Armpits/Genitals Thick/milky fluid Secrete into hair follicle Glands Aprocrine • Odorous, sweat-like material in armpits, navel, groin region, areolae • Inactive until puberty • Contain pheromones • Broken down by bacteria, creating odor Eccrine • Skin of armpits, foreheads, palms, soles • Mostly secrete water, w/ salts, organic compounds, and wastes (like urea) • Microbes feed on these as well, producing odors Specialized structures: • Hair follicle: cells of the epidermis extend into • • • • the dermis forming a small tube Hair bulb: base of the follicle Hair papilla: cluster of cells (live); nourished by BV’s Root: part of hair hidden in follicle Shaft: visible part of hair Sensory receptors • Communicate information from environment to the body • Found in all skin layers Mostly in innermost regions, fascia Free nerve endings/Nociceptor • Pain-sensing structures • Found throughout inner part of epidermis • Detect chemicals associated with tissue damage and bleeding Merkel cells • Sensitive to gentle physical sensation • Found in stratum germinativum • Abundant in fingertips Elongated, club-shaped pile of connective tissue Upper region of dermis (in dermal papilla) Respond to touch Look like onions Deeper parts of hypodermis Hard pressure, vibrations Pressure, constant touch Sensitive touch receptors Found mostly in mucous membrane of mouth Merely a keratin secretion Nail root • Lies beneath skin-nail fold • Grow back as long as nail root and skin-nail fold are not severely damaged • Grow 1/8 in per month Modified stratum corneum Grows from an individual follicle buried in subcutaneous layer Specialized Structures (continued) • Arrector pili: tiny, smooth muscle attached to base of dermal papillae & side of hair follicle Contracts: pulls on both simultaneously>>goose bumps What are the major roles of the integumentary system? What are “commensals”? How does heat regulation in the skin work? How does sensation in the skin work? Briefly describe the three classifications of burns Protection Heat regulation Sensation Waste excretion The skin protects from: • Chemical Damage Can break down connections between cells Can disintegrate cells Sweat dilutes & neutralizes Cerumen and sebum are oily barriers Repels water Repels dangerous chemicals that are dissolved in water Prevents water from escaping the body through the skin. The skin protects from: • Mechanical Damage Any type of force that can compress, erode, stretch or tear the skin. Loose connective tissue = flexibility Shedding stratum corneum = reduce erosion Calluses, adipose tissue and reticular fibers = shock absorption to minimize compression damage The skin protects from • Microorganism damage Produce destructive secretions in sebum / sweat Kept in check by chemicals that benefit commensals— ”good” bacteria and yeast that reduce the chance that harmful bacteria will survive on the skin. Shedding of stratum corneum removes microorganisms The body’s ability to maintain a constant internal temperature (98.6F) • Blood vessels contract / expand • Evaporation of the sweat from the surface • Adipose tissue is a natural “blanket” Sensation: received stimuli from the environment which is interpreted in a way that the brain can comprehend • Done by sensory nerves in the skin • Cold, heat, injury, pressure, stretching, touch • Transducers: nerve cells that convert various environmental messages into body signals. Eccrine sweat glands • Removes urea, organic chemicals, and excess salts • Not as efficient as the Excretory System Other functions • Vitamin D production when exposed to sunlight • Predictor of a person’s health Skin loses ability to maintain homeostasis locally and for the whole body Sun, cooking, acids, bases, corrosive chemicals, electricity, fires, and steam rooms Damage the skin differently Severity of burn is based on the extent of the skin damage. Reddening, swelling Superficial damage Steam, sun Damage to Strata spinosum & basale Blisters, reddening, swelling and fluid build up under the epidermis Entire epidermis affected, could be missing so stratum basale not available Damage to dermis: nerve cell loss Pain registers b/c histamine from immune system is released in response to the damage. Susceptible to dehydration, loss of body heat, and infection Skin entirely damaged; bone, muscle underlying skin damaged as well. (Too graphic to show) Guiding Questions: • What are the three major categories of disease in the integumentary system? • What are the various types of degenerative skin disorders? Genetic skin disorders? Infectious skin disorders? Degenerative • Progressive deterioration of tissue, environmental or physical stress Genetic • Mutations Infectious • Microorganisms that damage tissues and organs Solar lentigene • People in their 30s w/ overexposure Dermatitis • Cosmetics • Facial cleansers • Toners • Can accelerate skin aging Skin Cancer • Underlying genetic component—precancerous genes • If damaged, genes cause abnormal divisions of cells • Sun exposure Irregularly shaped black or brown spots that can develop into open sores • Injury deep in the skin Discolored blisters or sores Moles: flat squamous cell tumors Skin tags: soft knobby tumors that grow out of skin Seborrheic keratosis: Black to brown growth on face or body that creates a greasy, rough appearance to the skin Sebaceous hyperplasia: caused by oil glands, small yellow bumps with an opening in the middle Syringomas: sweat-gland duct tumor, small lumps on the cheeks and eyelids Lipomas: fat cell tumor, don’t cause problems normally Acne: stimulated by hormonal changes that cause and increase in sebum around the hair follicles. • Furuncle or boil: a buildup of dead cells and blood components caused by the inflammation of hair follicles. • Cysts or nodules: a sack-like structure filled with a fluid or semi-solid • Bacteria that feed on the acne pimple produce chemicals that aggravate acne Psoriasis • Increased amt of skin cell production • Causes a build up of thick scales on skin. • Unsightly, inflamed, painful, swollen Birthmarks • Port wine: begins at birth and grows, can bleed • Spider veins: central blood vessel with smaller vessels branching from it • Strawberry hemangiomas: enlarged blood vessels Vitiligo • Michael Jackson • White spots—hypopigmentation • Reduced melanocytes Albinism • No melanin production in the eyes, hair or skin Melasma • Brown patches on both sides of the face • Symmetrical • Does not completely disappear Staphylococcus aureus (bacteria) • destructive secretions that erodes and inflame the skin • Impetigo, SSSS, folliculitis Candida albicans (fungus) • Yeast in digestive system and female reproductive tract infect skin when immune system is compromised • Degrade tissue and cause inflammation More fungal infections = dermatophytes • Eat keratin-rich materials: hair, nails, and outer layers of epidermis • Itching, hair loss, deformation of nails • Ringworm (aka tinea) Contracted from furry pets Spread from one person to another through contact via clothes and skin Related to athlete’s foot or jock itch Warts (virus) • 60 types • HPV (human papilloma virus) Incurable Removal procedure Protists • Exotic tropical diseases that are spread by insect bites. • Can cause severe bodily damage if spread to internal organs Arthropods • Insects with exoskeletons, segmented bodies, jointed limbs • Follicle mite—undetected until inflammation of eyelash follicle occurs • Lice—blood sucking insects that irritate skin and spread infection as they feed Guiding Questions • What are “intrinsic” factors? How can they affect the skin’s aging? • What kinds of extrinsic factors can affect skin aging? • How does lifestyle accelerate skin aging? Extrinsic • Also external aging • Environmental factors: disease, pollution, sun Intrinsic • Natural maturation • Also internal aging • Accelerated by stress—pathology of other organ systems or environmental interactions Characteristics of skin aging • Loss of head hair • Graying and whitening of hair • Excessive growth of body and facial hair • Wrinkling • Drying of the skin due to diminished oil secretion • Skin sagging due to muscle atrophy • Regular irritation due to microbial population changes on the skin Impossible to stop • Natural decline of cells • Can be slowed by living in a mild environment • Elastin is naturally degraded by the dermis and subcutaneous layers Makes the skin less flexible, thinner, more brittle Decrease in blood flow slows cell division in basale & causes thinning of the epidermis More difficult to repair skin damage People with vascular diseases exhibit premature aging Decrease in melanocytes, nerves • More susceptible to environmental damage • Older skin can’t protect from UV and has difficulty registering injury. Susceptible to DNA damage • Oxidizing chemicals and sunlight • Cause cancers and tumors How to slow… • Diet, reducing exposure to UV, avoiding skin irritation, not smoking, protecting from air pollutants Smoking reduces blood flow to skin Can’t heal Decreases ability to maintain body’s temp Skin needling Promotes growth and swelling in wrinkled depression areas Makes skin smooth for a while • Take care of skin at a young age…difficult to reverse skin aging once the damage is done