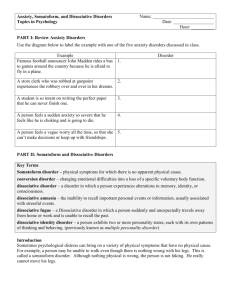
Somatic Symptom & Related Disorders and
advertisement
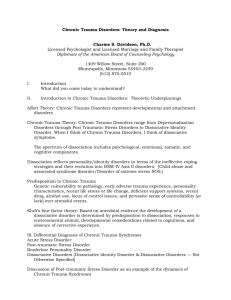
Chapter 6 Somatic Symptom & Related Disorders & Dissociative Disorders Somatic Symptom & Related Disorders Soma – Meaning Body Preoccupation with physical disorders Excessive or maladaptive response to or associated health concerns Includes the following 5 disorders: Somatic symptom disorder Illness anxiety disorder Psychological Factors affecting medical condition Conversion disorder Factitious disorder Somatic Symptom Disorder Illness Anxiety Disorder Formerly called “hypochondriasis” Physical symptoms are not presently experienced or are mild Severe anxiety about the possibility of having a serious disease Strong disease conviction Medical reassurance does not seem to help Illness Anxiety Disorder 1% to 5% 6.7% median rate of medical patients Causes Cognitive perceptual distortions Familial history of illness Treatment Challenge illness-related misinterpretations Provide more substantial and sensitive reassurance Stress management and coping strategies Conversion Disorder (Functional Neurological Symptom Disorder) Physical malfunctioning Lack physical or organic pathology Malfunctioning often involves sensorymotor areas Retain most normal functions, but lack awareness Freudian explanation Emphasis on the role of past trauma Not same as malingering (faking) Factitious Disorders Intentionally produced symptoms No obvious benefit Factitious disorder imposed on another’ known previously as Munchausen syndrome by proxy Intentionally produced symptoms in another person Dissociative Disorders Involve severe alterations or detachments Affects identity, memory, or consciousness Depersonalization – Distortion is perception of one’s own reality Derealization – Losing a sense of the external world Severe and frightening feelings of unreality and detachment Feelings dominate and interfere with life functioning Depersonalization-Derealization Disorder Facts and Statistics High comorbidity with anxiety and mood disorders Onset is typically around age 16 Usually runs a lifelong chronic course Causes Cognitive deficits in attention, short-term memory, spatial reasoning Such persons are easily distracted May begin with no trigger or stress/trauma Treatment Little is known Dissociative Amnesia Dissociative Amnesia Includes several forms of psychogenic memory loss Most common dissociative disorder Generalized vs. localized or selective type Dissociative Fugue (sub-type of dissociative amnesia) Take off and find themselves in a new place Unable to remember the past Unable to remember how they arrived at new location Often assume a new identity Dissociative Amnesia Usually begin in adulthood Show rapid onset and dissipation Occur most often in females Causes Little is known Trauma and stress can serve as triggers Treatment Most get better without treatment Most remember what they have forgotten Dissociative Identity Disorder (DID) Has at least 2 or more distinct identities (personality states) Identities display unique behaviors, voice, and posture Alters – Different identities or personalities Host – The identity that keeps other identities together Can it be faked? Hillside strangler case Controversial diagnosis Dissociative Identity Disorder (DID) Average number of identities is close to 15 (as many as 100) Ratio of females to males is high (9:1) Onset is almost always in childhood High comorbidity rates & lifelong, chronic course Considered rare Dissociative Identity Disorder (DID) Causes Histories of horrible, unspeakable, child abuse or other trauma Closely related to PTSD Mechanism to escape from the impact of trauma Treatment Focus is on reintegration of identities Identify and neutralize cues/triggers that provoke memories of trauma/dissociation