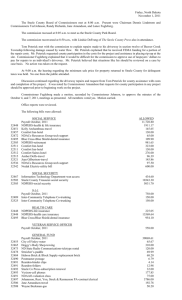
Prevention and Management of Aggressive
advertisement
Cynthia D. Steele, RN, MPH The Copper Ridge Institute The Johns Hopkins University Prevention and Management of Aggression Complex and difficult Support confidence and vigilance, not fear Provide skills and coach routinely Coaching means demonstration with the aggressive patient IF you are not willing to “get wet”, why should they? Loyalty and Support It is unacceptable to abuse residents and it is also inappropriate for you to be abused. We can solve the problems, but you must report it promptly after one incident Challenges Dementia units are the answer Victim blaming Turnover Transferring the patient Poor discharge instructions to the receiving staff Taking time to observe and be social first Lack of communication Create a common language and a Routine and safe place for reporting and discussing behaviors. The nurses “don’t ever listen” Be a coach and “get wet” If you are asking them to change their behavior, you must be willing to try it first. They will not believe you. The aides must not be routinely blamed. The Cynthia D. Steele, RN, MPH Caring Hands Award for Excellence in Care by Nursing Assistants, $1,000 award, recognition, status Recognize success, usually one person who “never has a problem” AD Uncomplicated, Complicated Categories of Misbehaviors Physical Verbal Sexual Exit seeking Others? Significance Common Alienation Risk of institutionalization Risk of discharge Increase in cost of care Caregivers Perspective Most common recipient Deliberate acts by a “bad patient” Random, unprovoked Tolerance varies greatly Demoralization Many belief systems A Dementia Sensitive Culture Educate everyone Use the same language Consistency of approach Confidence in ability to maintain safety Minimize impact of behavior problems Behavior Problems: and Risk Factors Cognitive impairment Psychiatric disorders Physical illness, Delirium Environmental press Caregiver approach *often multi-factorial Origins The 5 D Process Describe the behavior Decode it Design a plan Determine if it works Document, document, document Cognitive Risk Factors: The 4 A’s Amnesia: short term memory and learning Aphasia: communication Apraxia: coordination Agnosia: recognition Environmental risk factors Under/over stimulation Noise Activity of peers Cues and mis-cues Temperature Environmental Adaptation Shelter from chaos Structure, routine, familiarity Activity program Caregiver approach Miscommunication Rushing Threatening Inflexibility Too many persons talking and touching General Approaches Adjust expectations to abilities Identify and treat psychiatric conditions Give vigilant medical care Adjust environmental press Fine-tune caregiver approach Trial and error important Aggression Any behavior, physical or verbal that causes or has the potential to cause harm to self, others or objects “Handle with Care” Keenan and Steele, 1995 Cycle of escalation Response at each level Make a plan One person talking Safe Attire Body position Safe holds and releases Cycle of Escalation Calm Anxious Angry Hostile, threatening Aggression Micro-Cues Facial flushing Pacing Tension in muscles Gestures Response to Escalation Anxious Angry Hostile Aggression listen, comfort give space, monitor make a plan allow to defuse if safe, if not, use non-offensive physical control Make a Plan Communication essential Working together often more efficient Who will talk? Who will do care? Stance and Body Position 1) Relaxed posture 2) Eye level with the patient 3) “How-can-I-help” rather than “Youmust-do” 4) Body language should convey choices not control Safety Zone 1) Far enough away so you won’t get hurt… but 2) During care, you’re never in the safety zone! 3) Constant vigilance is required. Attire How you dress… 1) Avoid dangling hair, id tags, jewelry… 2) Wear footwear that favors movement. 3) Approaching patient? Remove glasses and watch High Risk Situations The Geri-Hold Common Examples Showering: Mrs. X due for shower Has hx of biting and kicking You reach across her to get the shampoo, she bites Exit seeking Mrs. R. sees you go out the door and attempts to follow you She says “I have to go to the bus stop for my kids” Dressing You tell Mr. G. to hold up his arms so you can pull over a sweatshirt He shoves you when you try to put the shirt on Transfers Mrs. X has just returned from her dental appt, She is sitting in a wheelchair and needs to be transferred to a geri chair or recliner She hits and kicks Approach to the Psychotic Patient Not useful Reality Often useful orientation Arguing Reasoning Threatening Empathy Reassurance Offering to help Distraction “Don’t sit on my Mother!” Not useful “There Often useful is no one here” “Just calm down” “What is upsetting you?” “May I sit down?” Remove the chair “I always wait for my husband to come home to eat!” Not helpful: Helpful: “You know he is dead” “I told you he isn’t coming” “You’d better eat or I’ll have to take the food away” “Let’s get started and I’ll watch for him” “I’ll keep a plate of food warm for him” “I am sure he is alright” Conclusions Caring for dementia clients is challenging Adjust expectations to abilities Use success of others Trial and error is important Joining “their world” can be fun