Experiences of neophyte therapy radiographers in extended role
Experiences of therapy radiographers in extended roles.
Angela Eddy
Senior Lecturer- Sheffield Hallam University
Background
Minimal empirical evidence around role extension/advanced/consultant practice in therapy.
Limited evidence around the process of learning and professional development (Donovan and Manning
2006).
Need to explore perceptions and experiences for new roles (Probst &Griffiths 2007)
Functioning in any new role is acknowledged as difficult and stressful (Johnstone 2007, Gerrish 2000)
Know that the transition experiences will be different to the experiences of those established in roles (Williamson 2006)
Research question:
What is the developmental process of the neophyte therapy radiographer working in an extended role?
Aims:
To examine the perceptions of therapy radiographers who have been working in extended roles for up to 2 years.
Gain an understanding of their professional development by exploring the nature and dynamics of the experiences that inform practice.
Objectives:
Undertake open interviews using grounded theory.
Develop a substantive theory which explicates the stages and processes of professional development for extended role therapy radiographers.
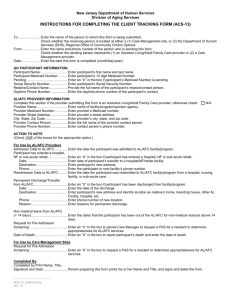
Name
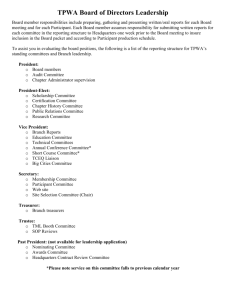
Story so far…10 interviews done
11 to go!
Role/scope of practice Length of time in Length of time qualified role
2.5 months 3 years Participant 1 Patient assessment and review.
Participant 2 Clinical trials/research.
3 months 16 years
Participant 3 Site specialist 2 years 34 years
Participant 4 Breast Mark up.
Participant 5 Site specialist
Participant 6 Patient assessment and review.
Participant 7 Site specialist
Participant 8 Site specialist
Participant 9 Site specialist
Participant 10 Breast Mark up
1year
18 months
18 months
2 years
6 months
2 years
3 months
4 years
2 years
35 years
14 years
4 years
25 years
20 years
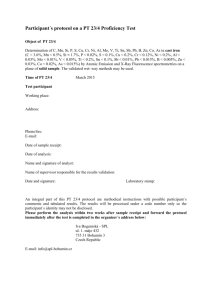
Early analysis and initial themes.
Name of code
Confidence
Mentors and role models
Frustrations/difficulties/ negative experiences
Transferable skills
Job satisfaction
Educational experience
Personal motivation/motivators
Time
Positive experiences/enablers
Communities of Practice
Working relationships
3
7
8
5
8
8
8
8
Sources
10
10
10
References
67
50
49
16
15
12
7
45
32
24
24
Development of Confidence is an overarching theme.
Links into other themes.
◦ What makes someone confident and how does that link into the stages and processes of professional development?
Professional confidence
◦ Task/role orientation and knowledge based skills.
Personal confidence
◦ Interpersonal and communication skills.
◦ Emotional intelligence (Goleman 1997)
Theoretical Framework
◦ Bandura “self efficacy” Framework (1982)
Banduras framework has four dimensions
What influences the development of confidence/ self efficacy ?
◦ Enactive mastery of experiences.
Learning the skills to perform in the role.
◦ Modelling.
Role models and mentors.
◦ Social persuasion.
Working environment, communities of practice.
◦ Physiological states.
Stress, anxiety, and “burn out”
Enactive mastery- skill acquisition
Clinical skills
◦ Development – stage progression to autonomy. Not having to refer on.
repetition and having done it time and time again so if you come across a problem you can recognise it”
◦ Underpinning knowledge – education
in the first year not to underestimate the knowledge required”
“ Even though I 've got a lot of years experience, having the M level study to underpin what I do gives me the confidence and I will argue the toss in a very confident manner"
Enactive mastery- skill acquisition
Leadership and management
◦
Some peoples leadership skills came from outside the
NHS or from previous experience as Supts.
◦
Learning and developing their own style:
“learnt not to impose, motivate rather than be dictatorial”
Interpersonal skills – working across boundaries
◦
“communication skills and negotiation”
◦
“ I deliberately don’t have an ego, and make sure I am seen to not be empire building”
Modeling – role models and mentors
Who were their role models and mentors:
◦
Mentorship/task and skill acquisition based assessments were done by Oncologists.
Case studies and problem based learning tasks
◦
However most had sought peer support and review from other professional groups:
“good ideas from other professions – we can be too insular”
“using clinical supervision with a nurse helped me to find the confidence to deal with difficult situations and anxious patients
Mentorship – what worked?
Challenging but supportive model in a time protected environment
◦
Someone who……“Would not stand over you and tut”
Identifying support and learning needs early in the process, not always easy
◦
" having come from a technical background to a very patient orientated background was quite a change for me so…..it was about having someone to talk to, and reflect on situations"
Social persuasion- developing a supportive learning community
Supportive working environment -
Communities of practice
Established teams in established roles
◦
“I enjoyed it because we could discuss things and it gave me confidence ”
Versus
Solitary role and a loss of identity
◦
“Feeling of professional isolation
”
Social persuasion – group working
Role of MDT’s
◦
“steep learning curve, thrown in at the deep end”
◦
"need to crack this relationship because its how the medical profession perceive you…its still a patriarchal system“
◦ Knowing the organisation – getting past information gatekeepers
◦
“working in a small department means I know everyone , not sure that’s the same in a bigger place“
◦
“wasted time, a lot of information is not shared – it’s a power thing”
Physiological states and stress /burn out
Personal resilience
In established roles:
◦
“actual transition into the role was straightforward
New Roles:
◦
“The first 6 months is a baptism of fire”
◦
“need to grow a second skin”
Moved along to by the end of the 2 year period
◦
“Not accepting boundaries” but felt burnt out.
Physiological states and stress /burn out
Role and scope of practice
No clear scope of practice… two perspectives:
◦
“that’s a good thing because I can shape the role” However….
◦
“if you are over ambitious its very easy to try and be involved in all bits but you cant do that”
◦
Role boundaries:
◦
“ tensions between Superintendents and us as they cant see where we fit, where their boundaries finish and ours start”
Physiological states and stress /burn out
Structure and organisation when implementing the role.
◦
“ had regular meetings and a structure and a plan with reviews built in”
◦
“3 months to get it organised and if I did not , it would be squashed”
◦
“Here is the key to your office, see you!”
Role security and sustainability of role
◦ concerns about long term career plans
◦
“Can this role be done by a nurse ”
So…..what are the stages and processes of professional development for extended role practitioners?
There maybe trigger points in the process.
Can there be one overarching process?
◦ It may be different depending on the nature of the role, the dynamics of the organisation and personal characteristics?
◦ Is there room for the development of a professional self assessment inventory which may help identify aspects of personal and professional development.
◦ Watch this space…………….