Elder Abuse at End of Life
advertisement
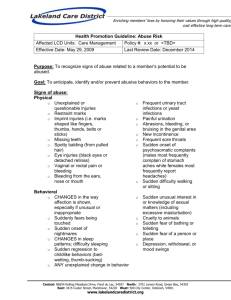
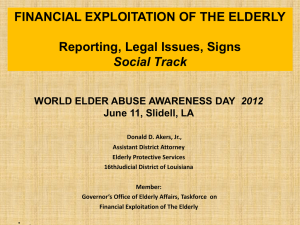
The Hidden Problem Abuse: physical, emotional, and sexual Neglect: self and other Exploitation: financial and sexual Abandonment No one knows for certain how big the problem is because relatively few cases are identified. It is estimated that 2 million older adults are mistreated each year in the U.S. 5 of 6 cases are NOT reported Hospice and palliative care patients have multiple risk factors o Dependent on others for care o Cognitive impairment o Caregiver stress Elder abuse can occur anywhere – in the home, nursing home, or other institutions It can affect the elderly across all socio-economic groups, cultures, and races Women and “older” elders are more likely to be victims Dementia is a significant risk factor Mental health and substance abuse issues are risk factors Isolation can also be a risk factor A Victim May… Have injuries that do not match the explanation of how they occurred and have repeated “accidental injuries” Appear to be isolated Say or hint feeling afraid, coded messages about what is occurring An Abuser May… Minimize or deny the victim’s injuries, attempt to convince others that the victim is incompetent or crazy, blame the victim for being clumsy or difficult Physically assault or threaten violence, prevent or forbid victim contact with others Act overly attentive towards the victim, especially in the presence of others A Victim May… Consider or attempt suicide An Abuser May… Consider or attempt suicide Have a history of substance abuse Have a history of substance abuse Be “difficult” or hard to get along with Refuse to allow an interview with the victim without being present, speak on behalf of the victim A Victim May… Be emotionally and/or financially dependent on the abuser Show signs of depression, stress, or trauma Have vague, chronic, nonspecific complaints An Abuser May… Be emotionally and/or financially dependent on the victim Turn family members against the victim, talk about the victim as though they are not there or not a person Say the victim is incompetent, unhealthy or crazy Why is this a bit tricky at end of life? Physical, behavioral, and emotional changes that happen at end of life may also be signs of possible abuse, neglect, or exploitation. Physical: slap marks, unexplained bruises, pressure marks, burns, blisters Neglect: pressure ulcers, filth, lack of medical care, malnutrition or dehydration Emotional: withdrawal from normal activities, unexplained changes in alertness or other unusual behavioral changes Sexual: bruises around the breasts or genital area and unexplained STDs Exploitation: sudden change in finances and accounts, altered wills and trusts, unusual band withdrawals, checks written as “loans” or “gifts”, loss of property Hospice Patient Increasing frailty Cognitive impairment Increased assist with ADLs Display of abusive behavior Unstable/poor social supports Conflicted relationships Caregiver Perception of stress Dependency on patient Poor relationship prior to illness Substance abuse Mental illness Burnout/frustrations Lack of skills Depletion of resources Educate ourselves and our team Increase communication among the hospice team to include each member’s observations and awareness when you suspect a situation. Our policy requires that our staff immediately report any suspected case of abuse, neglect, or exploitation to his/her immediate clinical supervisor or to the Clinical Counseling Officer. Remember that you don’t need proof of abuse, neglect, or exploitation to make a report – reasonable suspicion is all that is required Involving adult protective services does not mean your team failed Don’t assume that someone has already reported a suspicious situation. Most cases go unreported. Any individual who is legally mandated to report suspected abuse, neglect or exploitation and who intentionally fails to report such is guilty of a misdemeanor and liable for damages cause by failure. KRS Chapter 209 Lack of awareness of problem Insufficient understanding Loyalty to patient/family Legal and practical consequences Feeling of failure Assumptions about adult protective service response Denial of mistreatment Lack of recognition of warning signs Potential effect on rapport with patient and family Get management support Include team members and supervisors from the very beginning of seeing any of the warning signs Keep focus on enhancing quality patient care