Community Treatment Orders
advertisement
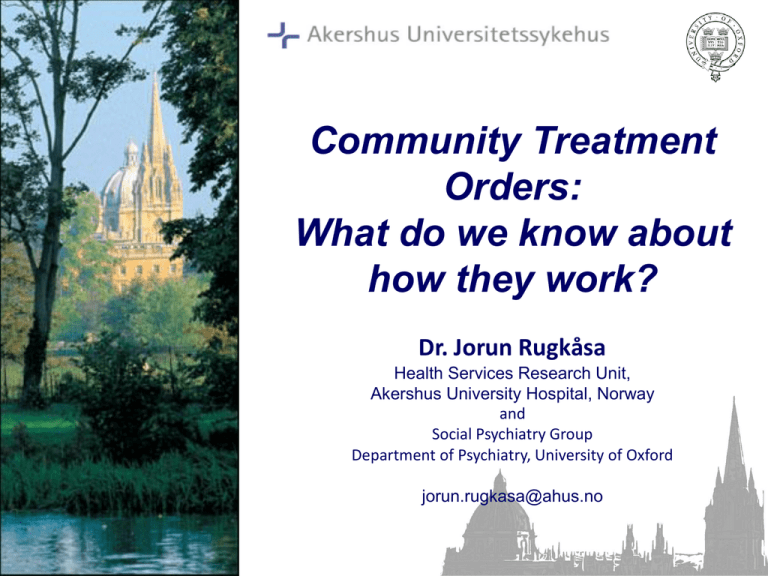
Community Treatment Orders: What do we know about how they work? Dr. Jorun Rugkåsa Health Services Research Unit, Akershus University Hospital, Norway and Social Psychiatry Group Department of Psychiatry, University of Oxford jorun.rugkasa@ahus.no Overview of presentation • Where do CTOs exist and how do they vary? • International data • What do we know about CTO effectiveness? • International evidence and systematic reviews • How are CTOs used in England & Wales over the first 4 years? • NHS data and survey of psychiatrists’ views and experiences Where do CTOs exist and how do they vary? Community treatment orders Canada Europe: Sweden, Scotland, England &Wales, Norway, Israel, some Swiss Cantons Australia USA (most states) New Zealand • Legal regimes allowing compulsory community supervision exist in ~70 jurisditions • Legal regimes vary, but overall, patients are obliged to adhere to treatment. Rapid recall • ’Outpatient committment’, ’Mandated Outpatient Treatment’, ’Community Treatment Orders’, ’Supervised Community Treatment’, ’TUD’ 1980s 1990s 2005 2008 1961 2001 OCT introduced in most north american states CTOs in Autralia and NZ Scotland England & Wales; Sweden } NORWAY TUD allowed in Norway TUD may be initiated from the community Some research conducted CTO discourse vs type of welfare state Country type Sweden Norway England/ Wales New York SocialSocialdemocratic democratic Liberal Liberal Controversy Some No Yes Yes Proceeded by high profile killings Yes No Yes Yes Evidence Agreement No Disagreement Disagreement Ideology Integration Treatment Protection Protection Control Broad Broad Risk Risk Patient rights Positive Positive Negative Negative Role in CTO discourse Adapted from: Sjöström et al., 2011 Issues that vary between CTO legislations • Whether CTOs may be introduced from the community or from involuntary hospitalisation • How they are linked to treatment/medication • The threshold for compulsion • Whether patients must have history of – Hospitalisation – Non-adherence • Rationale – Control risk – Provide alternative less restrictive than hospital Variation in use of CTO Between countries (in order of frequency) • Australia and NZ • England & Wales, Scotland • North America • In most (but not all) states there is a year on year increase (Lawton- Smith, 2005) • No reliable figures for Norway Within countries • Marked regional differences in many countries (including Norway) • Could be due to differing views among clinicians (Dawson 1995) • Might mean clinicans’ practice remains beyond the control of legislators (Sjöström, 2011) International evidence for CTO effectiveness Three key reviews of CTO evidence published → 2005 • Narrative Review: Dawson, J. (2005). Community treatment orders: International comparisons. Dunedin, New Zealand: University of Otago. • Systematic Review: Churchill, R., Owen, G., Hotopf, M. & Singh, S. (2007). International experiences of using community treatment orders. London: Department of Health and Institute of Psychiatry, King’s College London. • Cochrane Review: Kisely, S., Campbell, L. A. & Preston, N. (2005). Compulsory community and involuntary outpatient treatment for patients with severe mental health disorders. Cochrane database of systematic reviews, issue 3. Types of studies • Descriptive studies • Experimental studies • Experiential studies Descriptive studies Show remarkable consistent practice across jurisdictions: – Majority of patients are isolated, male, middleaged, schizophrenia, self-neglecting and lacking insight – High use of depot medication – Evidence of overuse – Evidence of increased level of overall coercion Current evidence on CTOs: Experimental studies • 2 case control studies – Western Australia and Canada – CTOs not shown to lead to better outcomes • Only two RCTs to date – Both in the US – No difference in primary outcome (readmission) in either study North Carolina secondary analyses (Swartz et al, 1999) • 57% reduction in means admissions, occupancy down 20 days (all) • 73% reduction in means admissions, occupancy down 28 days (schizophrenia) Experiential studies • Some good qualitative studies (though difficult to generalise across countries) – Doctors hold largely positive views – Families find them helpful – Patients are ambivalent • This literature is largely descriptive; little theorising around the issues Clinicians’ views of CTOs – More positive than patients – Yet law is insufficient to manage nonadherence – CTO involves tough choices, need to accept the role of the bad guy – CTOs are helping therapeutic relationships – Administratively burdensome – CTOs is a long term treatment form (O’Reilly et al 2006) Family’s views of CTOs – More positive than patients – CTOs provide support for patients – Grateful for police involvement but concerned about criminalisation of patient – Caregiving burden becomes more shared – But, family take the brunt of the burden when CTOs fail – Cumbersome administration weaken the efficiency of CTOs – CTOs need to be sustained (O’Reilly et al 2006) Patients’ views of CTOs – CTOs are coercive and appeals are futile – A contest of will and difficult to accept – Maintained for too long – Medication has side effects – Reluctant acceptance and recognition of a need for structure – Provide security and more freedom than hospitalisation – Doesn’t adversely affect therapeutic relationships (some variation here) – Some wish to remain on orders (O’Reilly et al 2006) Patients’ ambivalence • It was like a prison sentence. I could not go hunting in the forest with my sons. My psychiatrist was a fascist. The injections impair my alertness and energy. They took away my gun licence. • It brought me back into society as a normal dad. It lifted the burden of monitoring from my wife. It saved my marriage. It’s good but there’s handcuffs on it. (Gibbs, Dawson et al 2005) Coercion changes social status • Loss of credible identity • Changes to self image and presentation to others • Loss of autonomy • Feeling forced to “play the game” • Loss of trust in clinicians (Gault 2009) Temporal issues • “Thank-you-theory”: Patients are in retrospect grateful for coercive treatment • Little support for thank-you theory in the North Carolina RCT: most view CTO ambivalently and with little gratitude • However, those with good clinical outcome had more positive appraisal of CTO • Questions raised: – At what point does the patient express “real” attitude? – Does patients’ acceptance of force justify coercion? – We need a better understanding of patients as “moral agents” (Swartz et al 2003) 2005: the CTO evidence base is relatively weak • Systematic review of 72 published articles: ‘there is very little evidence to suggest that CTOs are associated with any positive outcomes’ Churchill et al., 2007 • Cochrane review of 2x RCTs: – 85 CTOs required to prevent one admission – 238 CTOs to prevent one arrest – Further RCTs urgently needed ‘they provide no significant evidence that CTOs affect health-service use, costs or forensic contacts.’ Kinsley et al., 2005 22 2005: the CTO evidence base is relatively weak – Early studies show reduction in readmission, but mostly poorly controlled; not conclusive – Later studies show more inconsistency re outcomes – Generalisibility issues • Discrepant methodologies • Different cultural/social settings – Uncertainty opens for different interpretations – All three reviews concluded RCT level evidence is needed CTO use in England, 2008-2011 CTO use to date • A 20 year debate produced strong opinions for and against CTOs • Govt’s guestimate for first year was ~400, but more than 4,000 were applied for • To date 10,000+ CTOs have been applied for • On 31st March 2011: – 4,291 people were subject to a CTO – 41.2% of CTOs have ended – 64% of CTO recalls result in revocation 25 CTOs: Total numbers, 2008-2011 Number of CTOs, recalls revocations and discharges, by year 2008/09 2009/10 2010/11 CTOs recall discharge revocation 2,134 207 33 143 4,103 1,207 1,010 779 Source: NHS Information Centre, 2011 http://www.ic.nhs.uk/ Total 3,834 10,071 1,601 3,025 1,167 2,210 1,018 1,940 Decrease in new CTOs of 6.6% from 2009/10 to 2010/11 Number of CTOs made and ended, by year Source: NHS Information Centre, 2011 http://www.ic.nhs.uk/ 27 The number of people on CTOs increased 29% from 2009/10 to 2010/11 Patients on CTOs at 31 March 2011 by gender Source: NHS Information Centre, 2011 http://www.ic.nhs.uk/ 28 Continuing slight increase in hospital detentions “In combination with the numbers of people on CTOs at 31st March 2011, it is apparent that increasing numbers of people are being subject to restrictions under the Mental Health Act.” NHS Information Centre, 2011, p. 19 29 How do patients get on a CTO? Source: CQC (2010). Monitoring the use of the MHA in 2009/10 NB: N= 208 Who are subject to a CTO? Source: CQC (2010). Monitoring the use of the MHA in 2009/10 NB: N= 208 CTOs and type of medication Source: CQC (2010). Monitoring the use of the MHA in 2009/10 NB: N= 193 (15 missing) Early indications • Pattern of CTO use seems to mirror the experience from other jurisdictions – Gender, diagnosis, medication usage, increased overall coercion • Early figures indicate varied practice – Great variation in use between NHS Trusts (N, and compared with use of formal admission) – Some RCs have not used any CTOs, some have used 20+ • Does the much higher number of CTOS than expected reflect – “defensive practice” – early perception of CTOs being effective? Clinicians’ views about CTOs 79 % Respondents 80 Crawford's UK survey 2000 (n=1171) 70 60 50 40 60 Molodynski UK survey 2010 (n=558) 46 35 30 20 10 18 9 1920 12 Dawson NZ survey , 2005 (n=284) 0 Prefer system Prefer system with CTO/in without favour CTO/against Unsure Manning et al, 2011 34 Conclusions • They are spreading across the Western, industrialised world. • Some variation, but in general obliges patients to adhere • Where do CTOs exist and how do they vary? • How are CTOs used in England & Wales over • Just like anywhere else the first 4 years? • What do we know about CTO effectiveness? • Not terribly much as there is no rigorous RCT (to be continued…)