Psychobiology
Research Group
Pharmacokinetics and
Phamacogenetics
Hamish McAllister-Williams
PhD, MD, FRCPsych
Reader in Clinical Psychopharmacology
Newcastle University
Hon. Consultant Psychiatrist
Regional Affective Disorders Service
Declaration of Interests
• I have received:
Speaker fees from:
• Astra Zeneca, BMS, Eli Lilly, GSK, Janssen-Cilag,
Lundbeck, Organon, Pfiser, Wyeth
Consultancy fees from:
• Astra Zeneca, BMS, Cyberonics, Eli Lilly, JanssenCilag, Lundbeck, Servier, Wyeth
Independent investigator led research support
from:
• Astra Zeneca, Eli Lilly and Wyeth
2
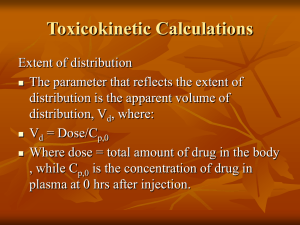
Pharmacokinetics
Barriers to drug delivery and effect
BBB or
other
Half-life
Volume of
distribution
Absorption
Membrane
transport
Dose
Clearance
Conc in
plasma
Conc in
target
organ
Effect
Pharmacodynamics:
-EC50, slope
-Effect delay
Membrane
transport
-Tolerance
First pass
metabolism
4
Pharmacokinetics and
Pharmacodynamics
5
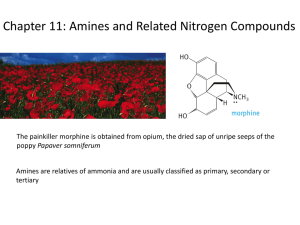
Pharmacokinetics
• Absorption
• Metabolism
• Elimination
General principles
Clinically relevant
examples
Theoretical plasma concentrations of three
drugs with different rates of absorption
1
AUC
Increased risk of toxicity
Plasma concentration
(proportion of dose)
0.8
Peak concentration (Cmax)
0.6
Minimum effective conc.
0.4
0.2
0
t max
Time
Absorption of TCAs
• tmax
tertiary amines:
secondary amines:
1 - 3 hours
4 - 8 hours
• Clinical relevance:
shorter tmax leads to higher Cmax
most side effects (e.g. sedation, postural
hypotension, membrane stabilisation) are
dependent on the plasma concentration
therefore give sedative TCA all in one dose at night
(and postural hypotension occurs while lying down!)
secondary amines often associated with fewer side
effects
Quetiapine IR vs XL
Datto et al. 2009 Clinical Therapeutics 31, 492
9
Quetiapine IR vs XL
Datto et al. 2009 Clinical Therapeutics 31, 492
10
Quetiapine IR vs XL
Datto et al. 2009 Clinical Therapeutics 31, 492
11
Quetiapine IR vs XL
Datto et al. 2009 Clinical Therapeutics 31, 492
12
Sedation with quetiapine IR and XL
Before treatment
Datto et al. 2009 Clinical Therapeutics 31, 492
After 5 days treatment
13
Drugs
15
Fluoxetine
16
Drug Metabolism
Type 1 metabolism
Cytochrome P450’s
Oxidation etc
Type 2 metabolism
Conjugation
Gluconurilation etc
Conjugation
O
Polar
species
Elimination
Non-polar
species
Biliary elimination
17
Metabolism of TCAs - 1
• Type 1 metabolism converts tertiary to secondary
amines, eg.
Amitriptyline
Imipramine
Clomipramine
Nortiptyline
Desipramine
Desmethylclomipramine
• Tertiary amines generally more potent 5-HT
uptake blockers, secondary amines more potent
NA uptake blockers
Up to 70% of clomipramine may be converted to
desmethylclomipramine
• may lead to lack of efficacy in OCD
Metabolism of fluoxetine
Cytochrome P450 2D6
Morphine
Morphine
glucuronate
19
http://medicine.iupui.edu/clinpharm/ddis
20
21
22
23
CYP 450 – 1A2 interaction examples
• Substrates:
Tertiary amine TCAs
Clozapine
• Inhibitors
Fluvoxamine, Ciprafloxacin
• Inducers
Brocolli, Brussel sprouts, tobacco, modafanil
24
CYP 450 – 2D6 interaction examples
• Substrates
TCAs, paroxetine, haloperidol, risperidone
• Inhibitors
Fluoxetine, paroxetine
Duloxetine
Cimetidine, sertraline
• Inducers
Dexamethasone
25
CYP 450 – 3A4,5,7 interaction examples
• Substrates
Many and varied drugs
Dexamethasone, tamoxifen
• Inducers
St John’s wort
Glucocorticoids
26
Elimination of drugs
• Primarily via the kidney
Metabolism of drug usually has to occur first to
produce a water soluble compound
This is usually the rate limiting step
Factors slowing metabolism will increase the
elimination time
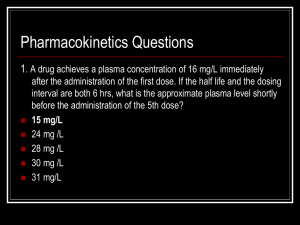
• Kinetics
Usually ‘first order’
Influences the dosing schedule
Influences the possibility of withdrawal problems
Plasma alcohol concentration (mg/dl)
Zero order kinetics
200
150
100
50
0
0
1
2
3
4
5
6
Time (hours)
7
8
9
10
• The rate of elimination
is independent of
plasma concentration
• A small change in dose
can produce a big
change in plasma
concentration
• Rare except if
elimination process is
saturated (can occur
with TCAs)
First order kinetics
Plasma warfarin concentration (ug/ml)
40
• The rate of elimination
is proportional to the
plasma concentration
• Elimination rate
quantified by ‘half life’
• The majority of drugs
have first order kinetics
30
20
10
t1/2
t1/2
0
0
10
20
30
40
50
Time (hours)
60
70
Theoretical plasma concentration of a first
order drug after single or repeated doses
Doses
Plasma Drug Concentration
(proportion of dose)
2
1
0
0
1
2
3
4
Time (number of half-lives)
5
6
Effect of reduced metabolism of a drug
on its steady state concentration
t
1/2
= 4 hours
(due to reduced
Plasma drug concentration
clearance)
t 1/2 = 2 hours
0
4
8
12
Time (hours)
16
20
24
Half lives of TCAs
Half Life
Metabolite
(hours - approx)
Amitriptyline
16
Nortriptyline
Imipramine
12
Desipramine
Clomipramine
18
DMC
Nortriptyline
60
Desipramine
50
DMC
45
Lofepramine
5
Desipramine
“…prescribing phenothiazines and tricyclic
antidepressants three times a day is
simply a public display of pharmacological
ignorance…”
R.E. Kendell (1993)
Companion to Psychiatric Studies, 5th Ed. p
419
Effect of varying dose and frequency
of administration of a first order drug
1.8
Increased risk of
side effects
Plasma drug concentration
1.6
1.4
Half dose,
1.2
twice as often
1
Control
0.8
0.6
Half dose,
0.4
same freq.
0.2
0
0
1
2
3
4
Time (number of half-lives)
5
6
Half lives of SSRIs - 1
Half life (hrs)
(Active metab.)
Fluoxetine
45-72 (150-200)
Sertraline
25 (66)
Citalopram
36 (?)
Paroxetine
10-20
Fluvoxamine
15
• Note inter-drug and
-individual variation
• Fluoxetine and paroxetine
t1/2 increases with dose
and time
Half lives of SSRIs - 2
Clinical Relevance
• Fluoxetine/norfluoxetine long half life
consequences:
5+ weeks to steady state
late emergence of plasma level dependent side effects
prolonged washout period
• N.B. delayed CYP2D6 inhibition
benefit for poor compliers
little risk of discontinuation syndrome
• Paroxetine short half life
SSRI most prone to discontinuation
• N.B. also anti-cholinergic
Pharmacokinetics Conclusions
• A knowledge of pharmacokinetics can improve
the clinical usage of drugs e.g. by:
minimising side effects associated with Cmax
• split dosages
• choice of drug (secondary versus tertiary TCA, IR vs XR)
adjusting dosages appropriately for age and sex
avoiding pharmacokinetic interactions
being aware of discontinuation phenomena