Clinical Sequelae of Child Trauma
advertisement
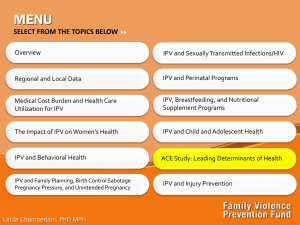
ADVERSE CHILD EXPERIENCES: Link Between Exposures and Health Nadine Burke Harris, MD, MPH CEO, Center for Youth Wellness April 10, 2013 CPMC Bayview Child Health Center The ACEs Study Vincent J. Felitti, MD and Robert J. Anda, MD, MS Asked 26,000 adults at Kaiser, San Diego’s Dept of Preventive Medicine. 17,421 participated in the study. Participants completed a questionnaire. ACEs Criteria 1. 2. 3. 4. 5. 6. 7. 8. 9. Recurrent physical abuse Recurrent emotional abuse Contact sexual abuse An alcohol or drug abuser in the household An incarcerated household member Someone who was chronically depressed, institutionalized, or suicidal Mother treated violently One or no parents, or parents divorced. Emotional or physical neglect Relative Risk of disease for ACEs ≥ 4 Hepatitis STD COPD Depression Suicidality 240% 250% 260% 460% 1,220% Mechanism Stress Response Activation of the HPA Axis - release of ACTH, adrenaline and cortisol Increase in centrally controlled peripheral sympathetic nervous system activity Activation of nor-adrenaline throughout the midbrain and forebrain including the cortex Multi-systemic Impacts Neurologic: HPA Axis Dysregulation Reward center dysregulation Hippocampal neurotoxicity Neurotransmitter and receptor dysregulation Immunologic Increased inflammatory mediators and markers of inflammation such as interleukins, TNF alpha, IFN-γ Multi-systemic Impacts Epigenetic Changes in the way DNA is read and expressed Changes in the way the brain responds to stress Endocrine Long-term levels. changes in ACTH, cortisol and adrenaline Updated Mechanism Positive Stress Tolerable Stress Toxic Stress Normal and essential part of healthy development Brief increases in heart rate and blood pressure Mild elevations in hormonal levels Example: Tough test at school. Playoff game. Body’s alert systems activated to a greater degree Activation is time-limited and buffered by caring adult relationships. Brain and organs recover Example: Death of a loved one, divorce, natural disaster Occurs with strong, frequent or prolonged adversity Disrupts brain architecture and other organ systems Increased risk of stressrelated disease and cognitive impairment Example: abuse, neglect, caregiver substance dependence or mental illness Intense, prolonged, repeated, unaddressed Social-Emotional buffering, Parental Resilience, Early Detection, Effective Intervention CPMC Bayview Child Health Center CPMC Bayview Child Health Center ACEs ≥ 1 67.2% ACEs ≥ 4 12% ACEs ≥ 4 and BMI ≥ 85% OR: 2.0 p< .02 OR: 32.6 p< .001 ACEs ≥ 4 and learning/beh probs N.J. Burke et al/ Child Abuse and Neglect 35(2011) 408-413 Effect of ACEs on Educational Outcomes SCOPE OF THE CHALLENGE Impacts are pervasive and long-lasting Development Physical and Mental Health Social and Educational impacts Economic impacts Prevalence is high Strong evidence relating the risk Early intervention improves outcomes PUBLIC HEALTH APPROACH IS NECESSARY What would it take? Align the activities of NIH, CDC, IOM, MCHB, ACF and CMS to provide the educational, financial, and logistical/administrative/systems support for: Basic science and translational research for the development of evidence-based practices, and Training for clinicians and researchers to develop and implement effective interventions. What would it take? Develop pediatric medical homes that are integrated both vertically and horizontally with the ability to provide: a) universal preventions to toxic stress, b) targeted, evidence-based interventions for those at risk for toxic stress, and c) evidence-based treatments for those symptomatic due to toxic stress) What We Can Do Now! Start Early! Identify kids exposed to ACEs through routine screenings and establish prevention programs in healthcare, schools and youth-serving organizations Focus on early childhood and early adolescence Critical developmental stages Invest in programs that heal Don’t spend money on programs that don’t support the health and development of our kids – punitive school discipline/juvenile justice What We Can Do Now! Change Public Policy Support prevention and healing using policy to prioritize funding for early detection and effective intervention Make ACEs a public issue. Educate our community about the impact and the role each of us can play. Center for Youth Wellness 22 Pediatric care Mental Health Community Education Data Gathering Seamless interaction CYW Case Management Training Analysis Best practice development Community Health and Wellness SOURCE: Core Team Research and Training Thank You! Resources Centers for Disease Control and Prevention UCSF Child Trauma Research Program http://childtrauma.ucsf.edu/ Lucile Packard Early Life Stress Program http://www.cdc.gov/ace/index.htm http://childpsychiatry.stanford.edu/clinical/stress.html National Child Traumatic Stress Network http://www.nctsn.org/ References “The Relationship of Adverse Childhood Experiences to Adult Health: Turning gold into lead” Felitti, VJ “Insights Into Causal Pathways for Ischemic Heart Disease: Adverse Childhood Experiences Study” Dong et al, Circulation. 2004;110:1761-1776 “Adverse Childhood Experiences and Chronic Obstructive Pulmonary Disease in Adults” Anda et al, Am J Prev Med. 2008 May; 34(5):396-403 “Stress Predicts Brain Changes in Children: A Pilot Longitudinal Study on Youth Stress, Posttraumatic Stress Disorder, and the Hippocampus” Carrion et al, Pediatrics 2007;119:509-516 “Adrenocorticotropic Hormone and Cortisol Plasma Levels Directly Correlate with Childhood Neglect and Depression Measures in Addicted Patients” Gerra et al, Addiction Biology, 13:95-104 “Adrenergic Receptor Regulation in Posttraumatic Stress Disorder” Perry et al, Advances is Psychiatry: Biological Assessment and Treatment of Post Traumatic Stress Disorder (EL Giller, Ed) American Psychiatric Press, Washington DC, 87-115, 1990 References Childhood maltreatment predicts adult inflammation in a life-course study Danese et al, PNAS, January 2007, 1319-1324 “Treatment o f Posttraumatic Stress Disorder in Postwar Kosovo High School Students Using Mind-Body Skills Groups: A Pilot Study” Gordon et al, Journal of Traumatic Stress, 17(2):143-147 “Mindfulness-Based Stress Reduction in Relation to Quality of Life, Mood, Symptoms of Stress, and Immune Parameters in Breast and Prostate Cancer Outpatients” Carlson et al, Psychosom Med. 2003 Jul-Aug; 65(4):571-81. “Usefulness of the transcendental meditation program in the treatment of patients with coronary artery disease.” Zamarra et al, Am J Card 1996 Apr 15;77(10):867-70 “Alterations in Brain and Immune Function Produced by Mindfulness Meditation” Davidson et al, Psychosomatic Medicine 65:564-570 (2003) Effect of buddhist meditation on serum cortisol and total protein levels, blood pressure, pulse rate, lung volume and reaction time. Sudsuang et al, Physiology & Behavior, Volume 50, Issue 3 September 1991, Pages 543-548