Case study of a patient with generalised anxiety disorder
advertisement
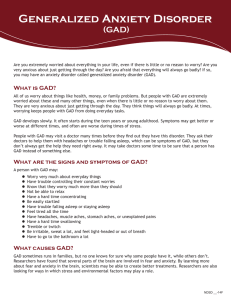
How to use Clinical Evidence to inform clinical decision making A case study using the CE review on generalised anxiety disorder Generalised anxiety disorder • Case history: 33-year-old man known to have GAD presents to you, his GP, with increasing anxiety. There is no specific trigger for, or focus to, his anxiety, but it is now present for a significant part of each day, and significantly affecting his life • He recognises his worries as irrational, but is unable to control the anxiety • He has presented to you and psychiatric services in the past with similar problems but says the situation has recently got worse History Case study constructed for purpose of Clinical Evidence demonstration. Not based on a patient seen by author, or on any particular individual • 33-year-old man, suffering from GAD for about 6 years • Past medical history – depression for 9 months several years ago • Family history – mother has depression, brother has alcohol dependence • Social history – recently started a new job working as a Sales Rep, involves driving daily for work, smokes 10 cigarettes per day, occasional moderate alcohol intake. Previously had a good social life with friends, now unable to socialise regularly due to GAD symptoms The patient’s concerns… • The patient explains he has tried diazepam before, and this had some beneficial effects on his anxiety, but it made him feel drowsy which means he could not drive • He would be interested to find out if there are other medications available, and is particularly concerned about becoming ‘addicted’ to any medications • He has found it difficult to take time off work to attend this appointment and doesn’t want to have to book more time off, as he does not want to have to explain to new work colleagues about this issue Issues to consider... • How can his anxiety levels be reduced? • SSRIs or benzodiazepines are commonly used treatments, but how useful are they? He has tried one drug in this class before, is it worth trying another one? What about the side effects? • Are there any non-pharmacological treatments that would help? • Which of these options are most appropriate for this particular person? • How strong is the evidence for these options? Where to start? • To use Clinical Evidence to find out what evidence is available on GAD, begin by going to the ‘Generalised anxiety disorder’ review on the Clinical Evidence website Further info on the condition, and on treatment guidelines available here Overview of the treatments for GAD, with their effectiveness rating, for easy comparison. Click on a treatment to see the evidence behind these categories These are the clinical questions we aim to answer. Navigation here if you just want to quickly browse selected parts of the background References here to related resources if you want further information, or more depth Now you have more background knowledge, look again at the interventions and their effectiveness. From the available evidence CBT appears to be Beneficial, antidepressants Likely to be beneficial, whereas other interventions are not From here, you decide to navigate on to CBT You have noticed that CBT appears to be Beneficial, a higher rating than other interventions. As the patient has no treatment preference you decide to find out more about the evidence base behind this, and begin by reading the Key Point Symptom severity is one of our outcomes of interest Navigating to the CBT page, we see the benefits and harms data. Systematic reviews or individual studies that meet our quality criteria and investigate clinically important outcomes are reported in the table The quality of the evidence is determined by the GRADE score Scrolling down this page, we see that relevant systematic reviews or RCTs each have a line in the table. The table summarises the population, outcome, results, and effect size, and indicates which intervention is favoured So CBT is compared against other interventions, but the outcomes of interest are the same throughout the review to ensure that you can assess consistently how each intervention compares and how it will help your patient Systematic review or RCT evidence is given the maximum score of 4 points Here we can see the total number of participants and studies that we have included for this outcome and comparison The overall GRADE score is obtained by adding the numbers in the row. 4 points is high-quality evidence, 3 points moderate, 2 points low, etc There are a variety of reasons why points may be deducted for quality, consistency, or directness reasons, and these are explained in the final column The GRADE table. This evaluates all the interventions we have included data on for GAD We have seen the benefits and harms of CBT compared with other interventions. Navigating back to the interventions table we can see what else is available, and how it is rated CE also includes a section on Updates and related articles on GAD CE also includes links to guidelines on the management of GAD. These are not limited to UK guidelines Patient concerns • This patient has concerns about medication affecting his ability to drive • He is worried that he may become addicted to medication • He is worried that the waiting list for CBT may take months • He is worried that attending CBT will mean he needs a lot of time off work. He wants to know more about CBT, however, and whether there are different approaches Dealing with concerns… • Do medications for GAD affect ability to drive? • We can go to the interventions table in the review and click on each of the medications to find out more. Unfortunately, all of the medications that are ‘Beneficial’ (antidepressants, buspirone, hydroxyzine, and pregabalin) can cause somnolence • Are medications for GAD addictive? • This isn’t covered by CE for most of the medications listed, as most of the RCTs we found did not cover long-term effects. However, we do point out that evidence from a non-systematic review showed that benzodiazepines produce dependence. We therefore need to look elsewhere for this information for the patient, bearing in mind what we know from CE about interpreting research findings Dealing with concerns… • What are the waiting lists like for CBT? • This is not covered by CE so we need to look elsewhere for this information • Do some psychological approaches need less time commitment than others? • In CE we cover CBT and applied relaxation. However, we do not comment specifically on how much time is needed for both techniques, so again we need to look elsewhere for this, bearing in mind what we know from CE about interpreting research Conclusions • We have used CE to learn more about the evidence behind different medical and psychological approaches to the management of GAD. • We have used CE to compare these interventions in terms of benefits and adverse effects • We can use this information, in conjunction with our knowledge of the patient’s condition and his preferences, to advise him on an appropriate treatment approach