Teaching Operating Room Conflict Management to Surgeons
advertisement

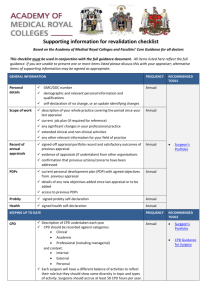
Teaching Operating Room Conflict Management to Surgeons: Defining the Educational Need and Identifying Effective Behaviors Association for Surgical Education March 24, 2012 Acknowledgements • Collaborators – Lorelei Lingard, PhD, University of Western Ontario – Sherry Espin, PhD, Ryerson University – Maggie Boehler, MS, Southern Illinois University – John Mellinger, MD, Georgia Health Sciences University – Nancy Schindler, MD, MHPE, University of Chicago – Mary Klingensmith, MD, Washington University – Jessica Davis, Southern Illinois University • Study participants Acknowledgements Funded by an Association for Surgical Education Foundation Center for Excellence in Surgical Education and Training grant Background Interpersonal conflict exists in the operating room and has consequences for team members and patients. Rogers DA, Lingard L. Surgeons managing conflict: A framework for understanding the challenge. J Am Coll of Surg 2006;203:568-74. Limitations • Research focused on communication, patient safety, human factors • Extent of and pathway to consequences not developed Rogers DA, Lingard L. Surgeons managing conflict: A framework for understanding the challenge. J Am Coll of Surg 2006;203:568-74. Study Goal • Clarify the specific educational need –Prior training –Conflict consequences • Identify effective behaviors –Allows an instructional target –Informs the development of assessment tools Data Collection and Analysis • • • • Five centers (IRB approved) Focus groups of OR nurses and surgeons Transcripts served as the data set Constructivist grounded theory processes Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative analysis 2006. Sage. Results • Thirty-one circulating room nurses in six focus groups • Thirty-five surgeons in six focus groups • Two hundred and twenty page transcript Needs Assessment • No formal educational preparation • Surgeons used trial and error of observed behaviors • Conflict and conflict management has consequences for surgeons, staff and patients Inadequate Training “I think the days of ‘I’m the surgeon...it’s my way and the rest of you be damned’ are gone. As the new younger people come out, while you may wish it may still be that way, you realize that it’s not.” (Surgeon, Institution B, 400.) Consequences for Team Members “You have a delicate, complicated operation you have to do and, you know, you have to focus all your concentration on that and you know if you have had a tussle with somebody it may make it difficult to do that.” (Surgeon, Institution E, 157.) Effective Behaviors Behavior Endorsed by both groups Forcing No Consistent with social science research Yes Maintaining calm Yes Yes Focused problem-solving Confronting Yes Yes Yes Yes Enhanced communication Yes Partially Forceful Responses “If I think that this person is not paying attention, I may have to raise my voice. I will later regret it. I will apologize and will later have counseling about it. But at the moment it was to save the patient.” (Surgeon, Institution E, 75.) Rogers DA, Lingard L, Boehler ML, Espin S, Klingensmith M, Mellinger JD, Schindler N. Teaching operating room conflict management to surgeons: clarifying the optimal approach. Med Educ 2011;45:939-45. Maintaining Calm “I guess one would be that if there is conflict that they are able to take control and put a hold on it…they are calmer and they are able to prioritize and rationalize important things instead of just flying off the handle.” (Nurse, Institution D, 83). Focused Problem-Solving • Concentrate on the immediate patient concern • Demonstrate flexibility about solutions • Appeal to administration about systems issues later Confronting “Well, I’ve confronted them before….I’ve had doctors and they come in carrying on ….and I’m looking at them and I just say, “We’re trying our best to do what we can do and some of the things are out of our control, but the things we can control, we’re taking care of.” (Nurse, Institution B, 239). Enhanced Communication “….if you slow things down and say ‘This is what you need to do, this is what is happening and this is what I want to do. Sometimes this helps.’” (Surgeon, Institution B, 242). Listening? “…I think as long as both people involved kind of acknowledge the option or input of the other person, sort of give them credit for saying like, oh that’s a good idea, or I see your point but this is my rationale for doing it this way…”(Nurse, Institution D, 176). Limitation • Hesitancy in sharing opinions • No follow-up sessions Summary • Compelling evidence of a specific educational need • Effective behaviors identified that inform development of a curriculum • Identified areas for future research Thanks Again! Funded by an ASE Foundation CESERT grant