Open Mind Presentation for Offender Managers
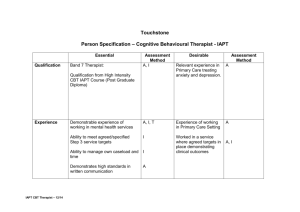
advertisement

IAPT Improving Access to Psychological Therapies Who are we?…..What do we do? Barbara Fulton, Lorraine Parker & Yvonne Drew Psychological Therapists: Open Mind Service Part of the wider NHS IAPT programme which implements guidelines for people suffering with depression and anxiety disorders We offer realistic and routine first-line psychological treatment Based at Cobden Street: our aim is to reduce barriers to accessing psychological treatment (that offenders may come across) Stepped care model Step 1: Recognition Step 2: Mild/Moderate common mental health problems Step 3: Moderate/Severe common mental health problems Step 4: Treatment resistant, Atypical and psychotic depression, psychotic illnesses, those at significant risk, Personality disorder Step 5: Risk to life, severe self-neglect Barriers • Blocking of Treatment (many offender service users have repeated experiences of refusal and exclusion from services) • Problems dismissed • Not registered with a GP Psychological Therapies A variety of therapies have been reviewed for their effectiveness (Nice Guidelines) CBT – depression & all anxiety disorders IPT, BCT, Counselling, BDT- depression (varying indications) CBT, EMDR- post traumatic stress disorder Cognitive Behavioural Therapy EMDR Barbara Fulton & Yvonne Drew Depression: Moderate to Severe Depression: Mild to Moderate Panic Disorder Generalised Anxiety Disorder Social Phobia OCD (Obsessive Compulsive Disorder) PTSD (Post Traumatic Stress Disorder) Hypochondriasis (Somatoform disorder) Specific Phobias Integrative Therapy Lorraine Parker Blends elements of a range of therapies - Gestalt - Object relations - Cognitive behavioural approaches - Attachment - Psychodynamic Personality disorder or characterlogical issues underlie depression and/or anxiety. Consider a referral if….. Depressed mood lasting for more than two weeks Anxious mood lasting for more than 2 weeks Has already been diagnosed with depression or an anxiety disorder Problem behaviour: which appears to be associated with anxiety or depression Sufficient time remaining: sentence/licence Not Offender Rehabilitation We specifically target depression & anxiety and not offending history We work within psychological models formulating the offender’s problems from their point of view Not about prosocial modelling, reinforcement and reward of prosocial behaviour Offending history is only focused on if identified as significant to their psychological problem and formulation Risk assessment and risk management throughout treatment Not offender Rehabilitation: case study Male, aged 45 Offence history: sexual relationship with a minor (15yrs), downloading & distributing images of children Unrepentant (makes this clear at initial meeting) Diagnosis: agoraphobia (since release from prison) Fear: “I could be chased, have to fight for my survival, do damage to my attackers and then end up back in prison” Problems identified: Isolated and depressed Therapy: Cognitive and behavioural interventions targeting avoidance of situations perceived as difficult to escape from Referral Process Provide the service user with information about IAPT Advise that therapy is not compulsory Complete referral documentation Questionnaire: this needs to be the service users interpretation of their mood and situation Service user needs to sign 2 consent forms (inc) Return the completed referral pack & book an available appointment slot IAPT staff are happy to guide you Referral Process 1st appointment: Initial assessment Assess for service suitability Assess for therapy suitability (CBT, EMDR or Integrative) Agree an initial treatment plan If not suitable: signposting/referral If not suitable: OM guidance Assessing for CBT Suitability why is this important? Service users with unfocused, multiple or very chronic problems are least likely to benefit from short term CBT Demoralisation CBT is not a one size fits all How OM’s can help with assessing suitability for CBT Is there potential for acceptance of the CBT model? “what are your beliefs about what’s causing your difficulties” Those with an insistence that their problem is due to a chemical imbalance or caused by other people are unlikely to be suitable How OM’s can help with assessing suitability for CBT Are the able to identify thoughts, feelings, behaviours and body sensations? Thought Body sensation Emotion behaviour How OM’s can help with assessing suitability for CBT Are they able to access their own emotions in relation to situations ? “how did you feel when that happened……” (look for a one word answer) Are they able to comment on their thoughts in relation to situations ? “what ran through your mind when that happened….” How OM’s can help with assessing suitability for CBT Are they goal orientated? …do they have the ability to work on one specific problem at a time? ….be aware of vagueness, rambling, frequent topic changes, desire to work on all problems at once How OM’s can help with assessing suitability for CBT Do they have alliance potential? - Note: eye contact, posture and general ‘feel’ - Poor rapport, idealising or blaming How OM’s can help with assessing suitability for CBT Are they able to accept personal responsibility in the therapeutic process? “what would you like to get out of therapy?....what might your role be in that” “you’d be expected to work on your problems in between cbt sessions….what’s your thoughts about that?” Active v Passive? Are they Anxious/Depressed……but struggling to meet the CBT checklist??? Seek IAPT guidance….. “It’s good to talk!” May be more suited for Integrative Therapy CBT checklist: the assumptions can be difficult to meet (those who Transference have PD or other characterlogical issues) Countertransference A redirection of feelings towards the service user Emotional entanglement with a service user Heart sink feeling….or hot potato Look out for: Service user reminds you of someone you have strong negative feelings towards Feeling parental towards them Overly identify with them Difficult to supervise/relationship breaking down Countertransference Is the service user wanting help with their anxiety or negative mood?....if not: Could the difficulties encountered be better dealt with in supervision with your manager Reflective and reflexive practice is key Be aware that countertransference is normal Be consistent with boundaries Co- existing Drug and Alcohol Use 70-80% of clients in drug and alcohol services have anxiety disorders, depression, trauma (Weaver, 2003) IAPT services should be working inclusively alongside substance misuse services to improve outcomes (IAPT Positive Practice Guidelines) CBT: Co-existing anxiety/depression (NICE guidelines (2007) Dug misuse: psychosocial Interventions) Co-existing Drug and Alcohol Use High Intensity Formal therapies delivered by IAPT therapist CBT for depression or specific anxiety disorder Low Intensity Delivered by IAPT therapist Guided self-help & Behavioural Activation for anxiety disorders and depression Low Intensity Delivered by Probation Key Worker Motivational Interviewing & Contingency Management Co-existing Drug and Alcohol Use No evidence that using substances makes usual psychological interventions ineffective Problem solving Time management Decision making Goal directed behaviour if an executive function deficit exists: CBT can be adapted Analytical thinking Executive Organisational ability Co-existing Drug and Alcohol Use Accepted: experimental, recreational as well as stable drug and alcohol use IAPT staff will determine stability Not accepted: unstable drug and alcohol use Instability across drug and alcohol use can lead to therapy disruption Multiple Competing Needs inc personality disorder, learning disability, drug dependence, alcohol dependence, homelessness, domestic violence etc............. • May lead to non attendance/disrupted therapy sessions /poor homework compliance • May compete with motivation for therapy and treatment engagement • Offender service users with multiple and competing needs may be misunderstood as being a ‘time wasters’ Thank You Any questions ………its good to talk!