Recognizing and Addressing Mental Health Issues in the EI Setting
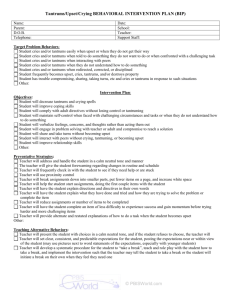
advertisement
1. 2. 3. 4. Recognize common behavioral/ mental issues in children Identify and differentiate between behavioral concerns and true developmental delays Recognize and understand the impact of familial mental health on children Identify and understand how to respond to common behavioral issues and when to refer. Temper Tantrums Noncompliance Aggression Anxiety Attachment Sleep Disturbance Temper Tantrums Aggression • duration • Intensity • Time of day • Setting • triggers • Impulsive • Anger vs. Communication Anxiety Attachment • triggers • Setting • Physical reactions • interaction • Family vs. public • Age of onset • Child history NonCompliance Sleep Disturbance • triggers • Setting – time of day • Setting limits/boundaries • Age • Frequency/external factors • Duration of sleep problems Conversation/observation is key in determining if behavior is typical or atypical. Here are a few things to observe: Duration – is the behavior lasting for long periods of time i.e. greater than 15-30 minutes Does behavior occur in a variety of settings? Is the child able to “self-calm”? Do triggers appear to be present? Is the behavior easily explained? Are there recent changes in the family? You determine the behavior present is not typical, what do you do now? Have a caring, supportive conversation with the family. Discuss with the family their concerns and ways you can help Assist the family in getting everyone “on board” with interventions Depending on the concern, refer to outside professionals **Interventions need to be addressed on IFSP** “Matthew” Matthew is a two year old boy who was initially referred to EI for speech concerns. At your last visit Mom tells the EI provider that Matthew’s temper tantrums are worse. Through conversation you learn that Matthew is having approximately 56 tantrums a day lasting 30 minutes or longer. Tantrums occur at home, the store etc. Along with his tantrums he is becoming aggressive. Mom has difficulty cooking dinner, shopping ,etc due to his increased tantrums. Do we address this concern on the IFSP? YES!! What does his IFSP look like? What are his outcomes? Who will provide the service? Outcomes need to be specific and functional for the family Procedures need to be specific for the family Services may need to be addressed as a non-EI service Depression Anxiety Personality Disorders Substance Abuse Major Mental Health Disorder Slow to respond to overtures for verbal or physical interactions by their children Make critical comments Have difficulty in encouraging the child’s speech/language facility. Have difficulty asserting authority and setting limits which would help the child learn to regulate his or her own behavior. Talk less to their infants Do use lilt and exaggeration that are typical of non-depressed mothers Less aware and responsive to their infant’s cues Have difficulty in providing appropriate stimulations. “Grace” Nine month-old “Grace” is listless. Referral information indicates she is not sitting up or pulling to a stand. What type of evaluations would you recommend based on this information? Typically this information would lend to PT evaluation…here is more information before we refer. Nine month-old “Grace” is listless. Referral information indicates she is not sitting up or pulling to a stand. Grace’s mother has frequent crying spells and spends little time with her infant. Left alone in her crib for long periods of time. Grace is unresponsive, difficult to arouse and looks downcast. Does this information change or alter our referral in any way? PT evaluation would be beneficial and necessary, however should not stand alone. Conversation with Mom and possible referral is vital. Routine Based Assessment is key in determining other causes to a child’s delay. When we evaluate the child, we need to look at the family as a whole Maternal Depression has been shown to be associated with the following: Increase in behavior problems Social-Emotional maladjustment Deficits in Cognitive functioning Difficulty with attachment Research has shown that if attachment is secure, the young child is more likely to successfully negotiate developmental tasks. Listen to the family – a good Routine Based Assessment will lead to discussion and help identify the parents concerns and possible behavior problems Focus on the issue – not the person. The child or parent is not “bad” – the behavior or behavior pattern is of concern. Be open and honest - ignoring issues will only lead to them becoming worse. Traditional behavioral interventions are not working Behavioral disruptions are occur in a variety of settings i.e. home, church, daycare etc. A person is at risk of harming themselves or someone else Suicidal ideations Behavior Problems in Children Licensed Counselor/Play Therapist who specializes in children Psychologist/Psychiatrist Local Mental Health Center Familial Mental Health Problems Licensed Counselor/Psychologist Substance Abuse Counselor/Group Local Mental Health Center Name/Number of local Crisis Line Behavior problems are common in toddlers Evaluate behavior to determine if it is typical or atypical Familial mental health is important, and left untreated directly affects the child Many behavior problems can be addressed on the IFSP, however it is important to know when to refer