PP_Z-Score_NFB_Insomnia_8-18
A New Look at an Old Workhorse: A Pilot Study of Z-Score Sensorimotor &
Individualized Neurofeedback
See full text at: Hammer, B.U., Colbert, A.P., Brown, K.A. and Ilioi, E. C. (2011).
Neurofeedback for Insomnia: A Pilot Study of Z-Score SMR and Individualized
Protocols. Appl. Psychophysiol Biofeedback, DOI 10.1007/s10484-011-9165-y
Email: barbhammer37@yahoo.com
Barbara U. Hammer, Ph.D., Agatha P. Colbert, MD, Kimberly A. Brown,
MSOM, Helfgott Research Institute, National College of Natural
Medicine, Portland, OR, Elena C. Ilioi, Psychology Honours, McGill
University, Montreal, Quebec, Canada
The authors are grateful to the Helfgott Research Institute of the National
College of Natural Medicine in Portland, Oregon for its generous support of this research. We are especially appreciative of the help from Mark L.
Smith and Nancy Wigton on the design of the protocols, William Gregory and Heather Jaskirat Wild for her assistance with the data analysis, and the generous support of our research assistants, Sean E. Griffith and
Tineke Malus. We thank all those who participated in this study, including those who took the time to complete the telephone screening and the extended screening sessions but who were not offered the opportunity to continue and to receive treatment.
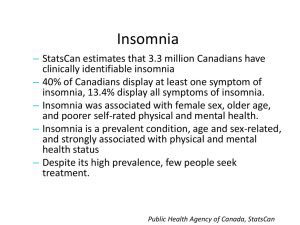
Insomnia Definition
Primary Insomnia (DSM 307.44): Complaints of Difficulty
Falling Asleep, Staying Asleep or Awakening too early, or
Non-restorative Sleep which occurs for at least one month and:
1. Causes significant distress or impairment in social, occupational, or other important areas of functioning.
2. Does not occur exclusively during the course of
Narcolepsy, Breathing-Related Disorder, Circadian Rhythm
Sleep Disorder or a Parasomnia.
3. Does not occur exclusively during the course of another mental disorder.
4. Is not due to the direct physiological effects of a substance or general medical condition .
2005 NIH Conference on Insomnia declared Insomnia an
Epidemic:
20-30% of adults in the U.S. suffer from Insomnia\
Insomnia associated with increased
Illness, accidents, healthcare utilization, and industrial expenses
Costs estimated at $14-80 billion annually
Pharmacotherapy limited due to negative side effects
• Psychological treatments
• highest co-morbidity
• Insomnia persists despite psychotherapy for depression or anxiety
• Cognitive Behavior Therapy —
• demonstrated 70% efficacy , effectiveness, efficiency for treatment of Insomnia but seldom used
• difficult to administer requiring specialized training/many sessions
• Challenges remain primarily in service delivery system. Internet based program promising
• Neurofeedback
• SMR from Sterman 1960’s to Hauri (1980’s)=cats to humans, improved sleep
• Theta benefitted tense insomniacs
• Individualized studied here
Peter Hauri (9/2008):
SMR Neurofeedback in 1980’s used Analog
Equipment not feasible for general clinical use:
Too Expensive
Too Cumbersome
Too Time consuming
Time to revisit SMR for Insomnia with Digital equipment and new training methods.
Pilot Study Overview: IRB approved 8/2008
Purpose –Compare treatment effects of Z score NFB SMR & sequential, quantitative EEG (sQEEG) guided
Individually Designed (IND) protocols for Rx of Insomnia.
Methods –Eight completed single-blind study.
Intervention –Fifteen 20-minute sessions Z-Score NFB.
Pre-treatment Screening—Medical History Questionnaire
Psychiatric Diagnostic Screening Inventory (PDSQ) plus:
Pre-post measures –
Insomnia Severity Index (ISI)
Pittsburgh Sleep Quality Index (PSQI)
Psychopathology (MMPI-2-RF)
Clinical Interview
Satisfaction/Happiness Quality of Life Index (QOLI) sQEEG
PARTICIPANTS:
25+ Telephone Screening –unpaid, recruited over 4 months
Exclusions —use of sleep aids, psychotropic meds, meds that impact sleep, mental disorders, physical disorders that could interfere, prior NFB, enrolled in another sleep study, pregnant or shift worker
12 Selected/Met DSM 307.44 criteria
2 Declined to start due to personal/extraneous reasons
2 Dropped out due to personal/external reasons >8 visits
Enrolled & Randomized (n=12)
Treated (n=10)
Excluded (n=10)
Not meeting inclusion criteria (n=3)
Declined to continue (n-2)
SMR
Allocated to intervention
(n=6)
Did not receive allocated intervention
(n=1)
Give reasons
Declined midway due to scheduling conflicts
Lost to follow-up (n=1)
Diqualified (n=1)
Discontinued (n=0)
Analyzed (n=5)
IND
Allocated to intervention
(n=4)
Did not receive allocated intervention
(n=1)
Give reasons
Declined midway due to scheduling conflicts
Lost to follow-up (n=1)
Diqualified (n=1)
Discontinued (n=0)
Analyzed (n=3)
Figure 1. STUDY FLOW CHART
Sleep Measures
ISI= Insomnia Severity Index--Perceived Severity of
Symptoms + Daytime Dysfunctions for past 1-2weeks
PSQI=Pittsburgh Sleep Quality Inventory--General Sleep
Disturbance + Daytime Dysfunctions for past 1month
Daily Sleep Diaries=from Screening Visits to Post Testing-recordings of bedtime, rising time, estimated latency, WASO, TST, Sleep Quality 1-10, adverse events or unusual circumstances
Actiwatch=72 hours pre and post treatment
Measures of Daytime Functioning
MMPI-2 RFMost widely researched, used measure of psychopathology. Newest version
Psychiatric Diagnostic ScreeningQuestionnaire-
PDSQ—Guide to depth clinical interview to confirm absent Dx
Quality of Life Index-QOLI— Measures positive mental health=daytime function
Objective Physiological Measures sQEEG=Quantitative Electroencephalogram
Profiles the brain’s electrical functioning in direct comparison with normative database (NeuroGuide).
Like other direct physiological measures, such as blood sugar, lipids or liver enzymes, the EEG has demonstrated high reliability
ActiwatchNumerous technical difficulties invalidated use
sQEEG—EEG General Screening
Records several minutes at 4 scalp sites in 5 runs for total of 19 of 10/20 sites
Records overall synchrony measures between each set of 4 sites
BrainMaster Certified Calibration tested EEG amplifier for NFB/QEEG
NFB=Operant Conditioning to Norm
Training to Norm =Normalizing physiological process via self-regulating brainwave distribution
Based on Principles of Learning via Operant
Conditioning
Z-Score NFB designed to use Live, Instantaneous record as basis of Reinforcement
Experimental Groups
Group 1—Z-Score Individualized Protocol (IND) =
Normalized 4 highest abnormal site(s) (HAS4) via reward of correct enhancement or inhibition of variables > ±1.96 Z , at increasingly larger percentage of normal Z scores. Modified
PZOKUL.
Group 2—Z-Score SMR Protocol (SMR) =
Training at Cz and C4, LE, reward production of SMR (12-15Hz)
& inhibition of excessive theta & high beta, & all other amplitudes & connectivity measures within normal. Modified
PZOKUL .
General Training Procedure =
I nitial % of all variables in the normal range =50% raised as %
Time >80 Z scores normal. When % variables >80, Z score limit was reduced as far as possible.
Table 1. Demographics, Complaints, Global Sleep Scores
3
4
Subject
Number
1
2
Age Sex Duration Symptoms Group Pre
ISI
61 F Since
Childhood
WASO,WE SMR 18
50 F 1-5 Years WASO SMR 15
5
6
34
40
54
50
M
M
F
F
5 Years
1 Year
SOL,WASO SMR
SOL,WASO SMR
7 58 F Since
Childhood
SOL,WASO
,WE
8 50
Mean 49.63
M 10+ Years NS,WASO,
WE
IND
19
17
20+ Years WE,WASO,
SOL
IND 14
22+ Years WE,SOL IND 12
SMR 28
14
17.13
Pre
PSQI
14
11
17
16
9
11
17
12
13.38
Note: WASO =Wake after sleep onset WE =Wake too early SOL =Sleep onset latency
NS =Non-restorative sleep, SMR =Z-Score SMR Neurofeedback IND =sQEEG guided individualized Z-Score protocol. These Pre-treatment ISI and PSQI scores are comparable to those of insomnia patients in other insomnia studies with larger patient samples ( Sleep ,
2005). ISI score range=0-28, PSQI score range =0-21, cutoff >5.
Success of Training
All subjects reached training goal of 80% correct within normal range for 80% of the training time.
Four of 5 in SMR improved SMR Zscores (toward 0) at training sites
ANOVA
Age, sex, PDSQ, Group not significant covariates.
Groups combined for all measures.
Pre-Post Significant Changes
Significant improvement on all primary sleep measures. See Table 2 &
3, Figs 2 & 3
Sleep Efficiency above diagnostic cutoff Post treatment
WASO significantly improved in half.
QOLI significantly improved
MMPI clinical improvement sQEEG significant lowering of Delta (sleepiness) & Beta (arousal) Table 4
Six month Follow-up
Six of 8 responded
Five of 6 remained free of insomnia, one returned to baseline, 3 improved from baseline
Table 2. Primary Sleep and Quality of Life Measures
Measure
ISI
PRE MEAN- (95% CI)
17.13– [15.794,18.466]
POST MEAN- (95% CI)
6.56 - [5.901, 7.220]
F
18.2 p
< .005
PSQI-T 13.38 – [12.506, 14.254] 4.50 - [4.194, 4.806] 55.6 <.0001
PSQI-SE –[74.85, 80.43] –
[91.87,94.49]
15.8 <.007
QOLI 46.13
–[42.908, 49.352] 52.63– [49.827, 55.433] 9.6 < .02
Notes: ISI =Insomnia severity index PSQI-T =Pittsburgh sleep quality index - total PSQI-SE= Pittsburgh sleep quality index total - sleep efficiency QOLI= Quality of life index. All measures are based on the eight completers. Lower ISI and PSQI total scores are better. Higher QOLI and PSQI-SE scores are better. Significant post-treatment improvement on all measures.
Table 3. Post Treatment Change Summary
#/ Group #Rx
Δ WASO
Final %ZOK Increase SE%
1-SMR 15 -1 80 7.2
0
2-SMR 9 95 14.3
-2
3-SMR 13 86 27.1
4-SMR 15
-3
90 23
5-IND 15
0
85 8.7
0
6-IND 15 93 7
0
7-SMR 15 87 28.6
-2
8-IND 15 88 11.1
Mean 88% +15.88%
Increase TST
’’
75
60
90
60
0
30
120
+61.88 Min.
60
Table 4. Binomial tests of sQEEG Changes Pre to Post Treatment
18
16
14
12
10
8
6
4
2
0
Pittsburgh Sleep Quality Index (PSQI)
PSQI Pre
PSQI Post
SMR-2 SMR-3 SMR-4 IND-1 IND-2 SMR-5 IND-3
Figure 2: PSQI Pre-Post Change in Global Sleep Scores
Figure 3: ISI Pre-Post Change
Figure 4: TST Pre-Post Change in Total Sleep Time
Actiwatch—72 Hour data pre-post with Multiple
Technical Difficulties Prevented Analysis
• Click sound inaudible
• Possibly defective recording hardware
• Possibly defective recording software
• Vender suggested corrections via Sleep Log questionable
• User errors discovered too late to re-train
Adverse Events
None reported
__________________________
Two drop-outs
Unexpected life-style changes (trauma induced) interfering with treatment schedule
Conclusions:
1. Baseline EEGs showed both excessive sleepiness and hyperarousal, which significantly improved posttreatment.
2. Both NFB protocols provided significant improvement in self reported sleep, daytime functioning, mental health, and sQEEG.
3. SMR treatment at least as effective as IND, and significantly less burdensome to administer.
Discussion
1) Data replicates early SMR studies with new equipment and advanced software/training designs
2) Z score NFB possibly effective at 8 Rx sessions (160”) training time, possibly faster than traditional NFB & CBT
3) SMR at least as effective as Individually designed protocol based on sQEEG
4) Participants improved on ALL self-report sleep measures, quality of life, and mental health
Discussion ( continued)
5) All Participants became normal sleepers, relatively quickly
6) Safe, well-tolerated, non-pharmacological,
Non-Invasive
7) SMR easily practiced clinically
Limitations:
1) Small Sample Size
2) Regression toward Mean
3) Lack of Control group
4) Single Blind Design
5) Lack of useful Actiwatch/objective sleep measure
6) Lack of EEG connectivity measures in IND