What is CAMHS and How do I Get It?
advertisement
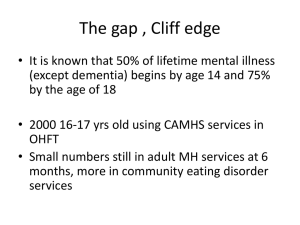
What is CAMHS and How do I Get It? Angie Davey – Primary Mental Health Specialist South Gloucestershire CAMHS - 01454 8632431 Aims Describing the S. Glos Child & Adolescent Mental Health Service To consider how the voluntary sector and CAMHS can fit together CAMHS thresholds Indicators of mental health concerns and risk Training available But First….. Who am I and why am I here? The S.Glos CAMHS team 9.8 Full time equivalent for up to 800 referrals a year Psychiatrists – currently locums Clinical Psychologists Family therapists Child Psychotherapist Consultant nurses – ASD and a Nurse prescriber Primary Mental Health Specialists – school age and pre school. Vacancy for ‘children living away from birth parents’ Barnardos participation worker Research tells us…. Three children in every classroom has a diagnosed mental health disorder One in five young adults shows signs of an eating disorder One in 12 deliberately harm themselves (and 25,000 of them are hospitalised each year because of this) Nearly 80,000 children and young people suffer from severe depression http://www.youngminds.org.uk/ To keep perspective…. many mental health difficulties are… Mild and transient – arising from combination of factors Reach a resolution with support and without an intervention from a tier 3 CAMHS service The episode is usually accompanied by psychological growth Indicators of mental health concerns Consider: Family and life context Mood Eating and drinking Sleep pattern Friendships/social activities School work Any safeguarding concerns? How have the above changed over time and what intervention has been tried (SAF (eh) assessment?) CAMHS thresholds (See full guidelines) Severe, complex and enduring mental heath difficulties where intervention at tier 1 & 2 i.e. community services has been attempted – (with a CAF/SAF(eh)) Such as: Risk of suicide/severe self-harm Severe depressive episode Psychosis Eating disorders ADHD/ASD with significant mental health difficulties Severe anxiety/phobic/panic disorders Gender identity struggles Complicated bereavement What is not an appropriate referral to CAMHS? Assessments for ADHD/ASD – Community Paediatrics Where a child’s difficulties are a response to normal life events Where difficulties are entirely school related Significant learning disabilities When intervention by tier 1 and 2 services has not been tried (through the CAF/SAF(eh) process) – unless there is a risk to life Urgency Checklist attempted suicide/ expressing thoughts of suicide? hears or sees things that do not exist? severe eating problems e.g. rapid weight loss (see full guidance) For an emergency mental health assessment – GP or A&E as appropriate (at Bristol Children’s hospital for under 16’s) What might increase concerns? Mood changes Difficulty sleeping Changes in eating, drinking, academic performance Changes in self-harm behaviours Expression and planning of suicidal intent Problems with drugs/alcohol use Break-up of a close relationship or major row Family history of self-harm, completed suicide Challenging behaviour or mental health disorder? ‘Conduct disorder where there is co-morbidity with other disorders and where specific intervention may influence outcome’ Pathway into CAMHS - some teams currently have a waiting list Further assessment/core work – within 10 weeks Opt in sent and choice appointment booked – within 8 weeks South Gloucestershire CAMHS Bristol CAMHS Tier 3 Single Point of Entry: Referrers may include GP Paediatrici an School Nurse Health Visitor Speech and Language Team Education, CYPS, Early Help process endorsed by Primary Mental Health Specialist Social Worker endorsed by Senior Prac or Team Manager What can the voluntary sector do? Think ‘family’ Think ‘multi-agency’ Support the SAF (eh) assessment and process Provide supporting information for a CAMHS referral Where there may be mental health risk – Child/young person to see GP Liaise with GP (with permission) Pass on safeguarding concerns Contact (child’s) local PMHS for advice Carry on what you are doing In conclusion: What makes a difference? Making sense of the difficulties developmentally and within their context – be curious Linking with school/social worker/other professionals involved Early intervention with community support Who needs the primary support - child/young person or their carers? A SAF (eh) to clearly identify needs Identifying risk and resilience factors clearly Passing on safeguarding concerns appropriately Acronyms explained ADHD – Attention deficit hyperactive disorder ASD/C – Autistic spectrum disorder/condition CAF – Common assessment framework CAMHS – Child and Adolescent Mental Health Service PMHS – Primary Mental Health Service SAF (eh) – Single assessment framework (early help) And other… Services available for Children and adolescents in need http://www.sgcyp.org/CommonAssessmentSupport/CAFToolkit/Resources/t abid/471/Default.aspx Training www.southglos.gov.uk/learning Mind Out – 1 day mental health awareness re school-aged children HRWorkforcedevelopment@southglos.gov.uk Early Attachment Relationships & Baby Brain Development (including trauma and loss): nancy.shelton@nbt.nhs.uk CAMHS Primary Infant Mental Health Specialist Social and Emotional Development of Infants &Young Children. 5 day course. Charges apply. jane.randall@nbt.nhs.uk Administrator Understanding Emotional & Mental Health in School-Age Children and Young People. 6 day training (Free for CCHP professionals otherwise charges apply) jane.clutterbuck@nbt.nhs.uk See: THANK YOU FOR LISTENING By Angie and Josh: Age 10 Any Questions?