By: Sarah Ake and Elizabeth Jubert
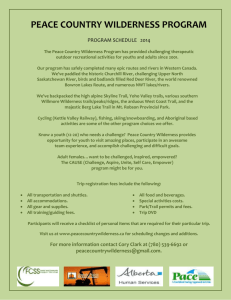
Utilizing outdoor challenges as a means for
therapeutic change, often in group settings.
Adolescents learn group dynamics,
wilderness skills, and outdoor living.
To build trust and self confidence in others and oneself using group
outdoor activities.
Includes group activities as well as solo self-reflective activities.
Catherine Freer Wilderness Therapy Program is designed to help “outof control” adolescents enable positive change. They incorporate three
models of wilderness therapy; a wilderness expedition, a school
combining academics and wilderness therapy, and a transitional home.
Catherine Freer Video
There are multiple exercises that are utilized in wilderness therapy
involving the establishment of trust and cooperation.
Here is one example!
The University of New Hampshire
has an Outdoor Education program.
UNH Outdoor Education Website
•Eating Disorders
•Substance Abuse
•Drug Abuse
•Behavioral Disorders
•Juvenile Delinquency
•Sexual Behavior Problems
1.
2.
3.
4.
5.
6.
7.
Gives the child the opportunity to experience successful coping
Reduce the potential risk factors impacting the child
Promote self-esteem and self-efficacy
Introduces positive opportunities for change and growth in a child’s life
Encourage positive processing of negative life events.
Hopefulness replaces helplessness.
A feeling of safety and security
1. Do not go into this work with Expectations of Successful Outcomes: It’s
okay to make mistakes and experience failures
2. “Warm up” Exercises are designed to help build comfort in doing this work
a. The Three T’s : Trust, Teamwork, Touch
3. Work in the Here-and-Now
4. The patient must have ultimate control; they can stop the exercise anytime
5. Don’t tell patients what to think, feel or do. Let them explore!
•The Use of Touch by Clinicians: More Hands on Contact with the Client than
Traditional Therapeutic Setting
•Confidentiality: Wilderness Programs must follow H.I.P.P.A which is difficult
in group settings with multiple treatment plans.
•Liabilities: Death and Injuries are more likely to happen in wilderness therapy.
Outdoor education teachers must pass State Board
examinations and follow standard education practices.
Psychologists must be licensed and maintain ethical
practices.
While a trip into the wilderness may be therapeutic it
is different than wilderness therapy. Wilderness
therapy has trained staff, licensed practitioners, and
individualized treatment plans to guide clients special
needs. Becker, 2009, p. 50
•Insurance Companies do not cover the costs of Wilderness Therapy.
•It is estimated that a year in wilderness therapy can cost up to $100,000:
Juvenile detention costs $48,000 in a year.
•Therefore, only those with higher SES can afford treatment.
•Outdoor Behavioral Healthcare
Industry Council (OBHIC): a panel
that searches for “best-practices” in
wilderness therapy and meets
required “ethical standards” .
•Mentors and role models for guidance
•Community resources : proximity to safe environments
•Family involvement
•Religious & Spiritual supports
•Meaningful role in community
•Access to recreational activities
•Possible family therapy, psycho-educational groups, and parent sessions
•Access to a school or learning community
If Wilderness therapy becomes more readily available and insured to lower
income families, then it may provide more relief to adolescents with a variety
of problems.
It will provide a more holistic way to achieving mental health.
It may reach children who would not thrive in traditional therapies.
More research will be available regarding the successes and efficacy of
wilderness therapy. And therefore, best practice standards can be developed.
More professionals will receive the appropriate trainings to provide these
more holistic approaches to larger groups of children and adolescents.
Becker, S. (2010). Wilderness therapy: Ethical considerations for
mental health professionals. Child & Youth Care Forum, 39(1), 47-61.
doi:10.1007/s10566-009-9085-7.
Longo, R. (2004). Using experiential exercises in treating adolescents
with sexual behavior problems. Sexual Addiction & Compulsivity, 11(4),
249-263. doi:10.1080/10720160490900623.
Scott, D., & Duerson, L. (2010). Continuing the discussion: A commentary
on “wilderness therapy: Ethical considerations for mental health
professionals.". Child & Youth Care Forum, 39(1), 63-68. doi:10.1007/s10566009-9090-x.
Ungar, M., Dumond, C., & McDonald, W. (2005). Risk, resilience and outdoor
programmes for at-risk children. Journal of Social Work, 5(3), 319-338.
doi:10.1177/1468017305058938.