Neurobiology-Informed Addiction Intervention and
Treatment:
Beyond PAWS
September 27, 2014
11:00-12:30pm
CEUH: NAADAC approved for 1.5hours
NAADAC continuing education provider:
# 549
Presenter: Joe Terhaar, Ph.D.
Location: Seattle
Course Description/Goals
Course Description: For each drug of abuse, Joe
Terhaar PhD will visually and kinesthetically describe the
impact on the brain, how the mechanical pattern of
addiction and craving develops, toward guiding the
practitioner in responding to the specific drug, increasing
motivation to abstain from drug use, stay engaged in
treatment, and empower recovery. The training will speak
to all chemical dependency counselor levels of knowledge
and skill in the neurobiology of addiction.
Course Goal: To improve the effectiveness of chemical
dependency counselors in motivating engagement and retention
of drug users in treatment with clear and specific information
about the compulsive impact of the drug on the brain and how
best to respond to each drug.
Participants will be able to:
Relate one salient emotion for each primary neurotransmitter of
drug abuse
Relate one salient neurobiological mechanism creating the
compulsive trap for each drug of abuse category, sufficient to
motivate behavior change
Detail at least one genetically mediated medical condition as a
parallel for understanding the predetermined trap of drug
addiction, and at least one genetic pattern increasing, and one
decreasing, the vulnerability to drug addiction
Specific to a drug, detail from the brain neurobiology one
adaptation to treatment that will increase the user’s motivation to
abstain
Joe Terhaar, Ph.D.
CAREER HIGHLIGHTS
Neurobiology-Informed responsive Addiction Treatment: One Therapist’s Experience. Advances in
Addiction & Recovery, Summer, 2014
*practicing licensed mental health counselor, marriage and family therapist, and certified chemical
dependency counselor for over 30 years with experience in drug prevention, intervention, and
treatment;
*Full Member of the Association of Intervention Specialists, a contiguously Board Registered
Interventionist-I and subsequent Certified Intervention Professional using nine strategies in helping
families motivate their loved-one to enter treatment;
*presenter of Neurobiology-Informed Addiction Intervention and Treatment, at the Association of
Intervention Specialists Fall Conference, Palm Desert, California in October of 2013 and the
NAADAC National Conference in Seattle in September, 2014
*expert witness for courts litigating issues of addiction diagnosis and family intervention practices;
*awarded a rare dissertation research grant to study family intervention by the National Institute on
Drug Abuse (NIDA) National Institutes of Health in 2001 contributing to the science of family
intervention;
*state-approved marriage and family licensure supervisor since 2008;
*author and former provisional patent holder of research-grounded concepts, skills, and objectives for
the articulation of family intervention;
*Who's Who Among Students In American Colleges and Universities, 1976-77;
*author of training curricula for school teachers, social workers, and drug counselors adopted across
the U.S. from Seattle to Georgia; author and manager of over $250,000 in grants and contracts
Outline of Training
Intro
Overview and Goal: Replace denial with neuro awareness
Toward:
Intervention: Motivate engagement in treatment with
awareness of trap
Finlay (1966) said “concern for self,” bring to focus the
reasons for concern
Empower families and the addict through neurobio
Adapt intervention process with awareness of neurobio
Inform all of the trap that will result in fatality
Counselors who briefly explain the
impact of the drug on the user’s
brain—providing the opportunity to
understand what is currently driving
the behavior—free the family from
acting on misguided guilt and grief,
toward proactive interventions that
preserve life.
Genetics To Reduce Misdirected Guilt
(Refer to Video and provided handout)
If confront denial alone: this risks
being oppressive and negating the other
aspects
Bio/psycho/social: but let’s look at
massive impact of genetics and neuro
Neurobiology for Motivation and Treatment
Stimulants and Methamphetamine
Review personalities of brain neurotransmitters (Handout)
(action of ntr vs location)
Impact: on ntr: immediate DA (NA), 5HT (RN), NE (LC), sex,
Lisa on North side: exhausted and depleted
Karen on south hill: got up to eat; depleted
Crave cycle: A-VTA-NA (For 2-3 months after last use, higher Δ Fos B
with lower DA in NA appears to explain 25% of the chronic cocaineinduced changes in gene expression and craving; thus a pattern of craving.)
Crave: foil, glassware, etc.
The paradox for the 9-repeat user
Motivation: Show trap
Motivate by showing the depletion and
desperation; loss of pleasure (ntr)
Get them while they are depressed
Inpatient support if unstable
Cut off the money
From, “Your in denial” to “You are
trapped and we can help you get out”
Treatment: do not do grief work
*Structure/support and over Grief
Ethanol
The critical roles of
DA & glutamate,
B-endorphin & naltrexone (less reward from drinking),
serotonin
GABA and anxiety in LC
(about motivating family and drug users, not
psychopharm class)
Motivation: Show trap especially of 5HT
Motivate from his/her loss
of contentment
(low 5HT): SLC6A4; they are afraid to act, reassure of
contentment (Bill in hot July; Norm: loss of
contentment)
Get them while they are depressed,
but caution
of anxiety (LC-GABA)
Concern for self: Physical deterioration and need for physical exam
Risk of seizures with abstinence: benzo for travel: family talk to doc
Treatment: Craving and Physical rehab
Structure & Grief: Cuing system is strong, must interrupt crave cycle, other
family alcoholics keeping family norms of us
* Orange Julius gal: triggered by my orange juice
Physical rehab: diet supplements: beCalm'd, Neu-be calm'd); good
nutrition due to malnutrition
Medications: Vivitrol/ReVia,
Check other meds
Case study: RLS: Mirapex (Pramipexole) is a Dopamine3 agonist and
rebalances the balance reducing sx of RLS; but also triggers compulsive
gambling, sex, stereotypy, and overeating in 14% of individuals, likely from
triggering striatum; Joey: was it only DA3 behavior or addiction exacerbated
by D3 trigger?
CNS depressants
The critical role of Benzo:
suppress locus coeruleus and reduce anx until
withdrawal
Withdrawal risks GABAA and Cl-, massive anxiety
GABA anxiety without coping capacity
Go to treatment so you do not have to be so anxious
The critical role of Benzo weakens regulatory capacity
of the VTA and permits excess DA (pleasure)
Motivation: Show trap especially of GABA
Concern for self: anxiety without coping capacity (student Amanda)
Kid unable to pee due to anx; Northern nurse (tritrate)
Anxiety vs no motivation
Risk of anxiety and seizures with abstinence: benzo for travel
Withdrawal varies due to length of use: 40-45% who
use more than 4 months have physical dependence; 80 to
85 % if more than 2 years.
Treatment: Craving and Physical
rehab
Structure & Grief: Cuing system is
strong, must interrupt crave cycle
Support small reward pattern for
forward movement; structure reward
system for action and specific tasks
Support later grief of lost aspirations,
once stable in abstinence
Opioids
Mimics natural endorphins that reduce transmission of
substance P to dull the perception of stress from pain via the
locus coeruleus; strong stimulation of mu to increase
dopamine activity, strong anticholinergia from suppression
of NE in the locus coeruleus (suppressing alertness and capacity
to express adrenaline) causing somnolence; opioids stimulate
glutamate receptors enhancing the pleasure of DA.
Phil’s hand: 20/80%
b. craving cycle A-VTA-NA
Tramadol itself does not trigger μopioid receptor, but is metabolized to
O-desmethyltramadol, a significantly
more potent μ-opioid agonist, creating
euphoria and craving
c.
Motivation: Show trap of running
from pain
Concern for self: always trying to
outrun the pain
(Annie to LVRC; Asian Tom for suboxone)
Comfort of pleasure, fear of pain
Ease withdrawal with buprenorphine
Loss of comfort and contentment:
cannot appreciate the sun
Treatment: Craving and Physical
rehab
Structure & Grief: Cuing system is
strong; interrupt crave cycle
Support dealing with natural pain of
daily life
Support later grief of lost aspirations,
once stable in abstinence
Pain
For some, short acting opioids inflame glial cells in the
spinal column amplifying and perhaps initiating
neuropathic pain.
Motivation: Reflect the loss of pleasure to avoid pain and
regain happiness by effective pain treatment. Validate pain as
real (with or without primary injury); explain pain mechanism
and relief of better pain treatment (Ashley; Bill from north
county with st hernia)
Treatment: 10 non-opioid pain management strategies
integrated into daily life at Las Vegas Recovery Center
Buprenorphine
Suboxone, Subutex: dysphoria in last
stage of stepdown: glutamate, serotonin,
dopamine
Intervention: detox from buprenorphine
Treatment:
Apt substitute for short acting opioid
for pain patients in recovery or chronic
pain patients
Inhalants
Disrupt DA in VTA and NA, (pleasure) and
GABA (anxiety)
De-myelination of the neuronal sheath resulting
in dementia. Likely has connection to NMDA
and DA thus psychosis and euphoria.
Motivation: Risk of volatile behavior and
denial of problem
Concern for self: brain damage
Anxiety vs no motivation
(2010) Gruber found chronic users experienced
deficits in “cognitive flexibility” making continuing
the same mistakes even when corrected. Also seen
were those smoking earlier and longer experienced
greater deficits. Bolla et al. (2002) found that effects
last 30 days or more after use.
Treatment: Craving and Physical rehab
Structure & Grief: Cuing system is strong,
must interrupt crave cycle,
structure to avert cravings
brain damage risk requires special education
assessment for learning support educationally.
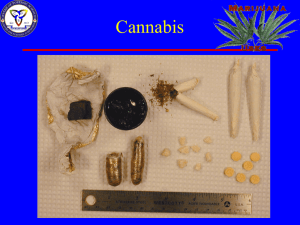
Cannabis
CB-1 and anandamide:
reduced ACH in hippocampus= reduced memory
likely with
reduced glutamate (reduced excitation) and
sidestep hypothalamus (reduced anxiety) and
inhibit GABA (inhibitory) in pons and amygdala
Via anandamide, increased DA in NA probably from
VTA
Thus, pleasurable to have low physical response capacity
while perceiving everything as pleasurable and interesting
and not record anxiety not felt, thus no reason to challenge
self or change:
trick brain into feeling that the mundane is
enjoyable and interesting, stealing motivation to plan,
act, move forward or especially risk something new and
challenging
Rare psychosis risk due to glutaminergic
NMDA for a few.
Camaraderie of cannabis: amygdala larger
with larger and more complex social
networks
Motivation: lack of motivation
Call withdrawal what it is, if recently abstinent
Drug user is not accustomed to taking initiative and
moving beyond anxiety, but needs to for
treatment; address lost aspirations and
encourage reconsidering goals; rebound anxiety
Support resuming aspirations with initiative for
abstinence
reatment: lack of motivation
Concern for self: brain damage; loss
of aspirations
Anxiety vs no motivation
T
Psychedelics
LSD
1. LSD & psilocybin: serotonin agonists, reducing
serotonin action at postsynapse; binds to serotonin2A sites,
triggering other neurotransmitters. Also, altered action of
glutamate and DA in the raphe nuclei. Mescaline has
greater proportional effects on norepinephrine, and
perhaps dopamine and serotonin at high doses. Some mild
ACH effects.
2. Motivation: Same as cannabis and MDMA.
3. Treatment: Same as cannabis and MDMA.
Anticholinergics
(scopolamine, belladona, atropine, hyoscamine, plants like
Mandragora officeinarum) or in Jimsonweed (Datura
stramonium): Dryness creates a delirium with mild euphoria
2. Motivation: Same as cannabis and MDMA.
3. Treatment: Same as cannabis and MDMA.
Glutamic: PCP, K,
Triggers NMDA-type glutamate receptors (of DA and NE)
by blocking calcium flow with interaction between
dopaminergic and glutaminergic neurons. In higher doses,
may also affect 5HT
2. Motivation: Same as cannabis and MDMA
3. Treatment: Same as cannabis and MDMA
MDMA
Loser doses it acts like serotonin; higher doses like
amphetamine
2. Motivation: Same as cannabis and MDMA
3. Treatment: Same as cannabis and MDMA
DXM (dextromethorphan)
An opioid-like drug that binds to and acts as antagonist to the
NMDA glutaminergic receptor
Motivation: Same as cannabis and MDMA
Treatment: Same as cannabis and MDMA
Joe Terhaar, Ph.D., LMFT, LMHC, AIS, CIP
Intervention Specialists, LLC
9203 E. Trent, #2
Spokane WA 99206
509-838-2111
866-788-7464
www.TreatWithCare.com
To order the DVD for neuro motivation in your
sessions, go online to:
www.SilvertopVideo.com
And pay only $150 with the NAADAC conference
discount