Manual Jimenez
advertisement
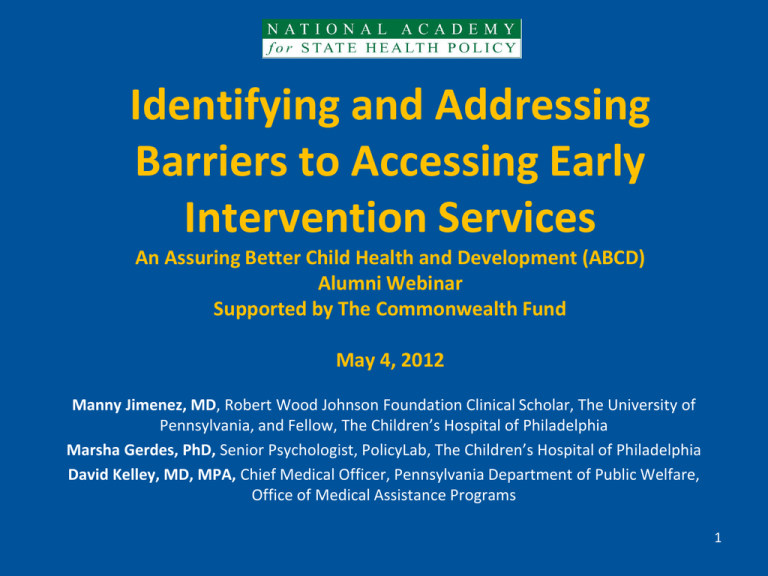
Identifying and Addressing Barriers to Accessing Early Intervention Services An Assuring Better Child Health and Development (ABCD) Alumni Webinar Supported by The Commonwealth Fund May 4, 2012 Manny Jimenez, MD, Robert Wood Johnson Foundation Clinical Scholar, The University of Pennsylvania, and Fellow, The Children’s Hospital of Philadelphia Marsha Gerdes, PhD, Senior Psychologist, PolicyLab, The Children’s Hospital of Philadelphia David Kelley, MD, MPA, Chief Medical Officer, Pennsylvania Department of Public Welfare, Office of Medical Assistance Programs 1 Overview • Barriers to Early Intervention Services (Manny Jimenez) • Understanding Barriers to Services (Marsha Gerdes) • CHIPRA Quality Demonstration Grant and Pennsylvania’s Early Intervention Strategies (David Kelley) • Current Successes and Challenges (Marsha Gerdes) • Facilitated Discussion (Jill Rosenthal) 2 Disclosures • Manny Jimenez’s work was supported by – The Robert Wood Johnson Foundation Clinical Scholars Program at the University of Pennsylvania – A 2011 Academic Pediatric Association (APA) Young Investigator Award (YIA) for Child Development and Preventive Care Services for Children, Ages 0-5, supported by The Commonwealth Fund • No conflicts of interest 3 Problem • Part C of the Individuals with Disabilities Education Act mandates early intervention (EI) for infants and toddlers with developmental delay • AAP advocates for early identification • 13% of infants and toddlers have developmental delays that qualify for EI services. • 90 % of eligible children do not receive EI services. 4 Path to EI Evaluation from Pediatrician’s Office Health care provider identifies developmental concern at well child visit Provider conveys concern to parent Health care provider refers patient to EI Option 1Physician faxes Evaluation Contact with EI intake staff referral form Meeting with service coordinator appointment arranged Multidisciplinary evaluation Option 2Physician gives parent EI phone number Parent agrees to call EI Parent makes phone call 5 TEDS Study • Translating Evidence-Based Developmental Screening (TEDS) into Pediatric Primary Care – December 2008 through June 2010 – CDC-funded randomized controlled trial of developmental screening in four urban, primary care practices – 2092 children age 0-36 mos – 332 children referred to EI – 162 Not Evaluated by Early Intervention 6 Goal To understand why infants and toddlers referred to EI are not always evaluated from the perspective of parents and EI employees 7 Data • Interviews with – 22 Parents of infants and toddlers referred to EI and not evaluated – 22 Parents of infants and toddlers referred to EI and who were evaluated – 14 EI Employees (Intake staff and service coordinators) 8 Parent Participant Characteristics Evaluated by EI (n=22) Not Evaluated by EI (n=22) Parent Age Years Parent Race African American Caucasian Asian Other Ethnicity Latino Non- Latino Parent Education Some College or > 30.8 (21-45) 28.5 (22-36) 13 (59.1%) 6 (27.3%) 1 (4.6%) 2 (9.1%) 17 (77.3%) 2 (9.1%) 1 (4.6%) 2 (9.1%) 1 (4.6%) 21(95.4%) 3 (13.6%) 19 (86.4%) 14 (63.6%) 12 (54.5%) Employment Unemployed 15 (68.2%) 13 (59.1%) Income <33,000 10 (45.5%) 13 (59.1%) 9 Themes • • • • • Miscommunication Parents Want to be Heard Parental Wait and See Practical barriers Skepticism 10 Miscommunication • Hearing reassurance rather than action is necessary 11 Communication Problems "I was voicing my concerns...she agreed with them but didn’t seem overly concerned, so that kind of brought me down a few notches and so my urgency was already dropping at that point. So I didn’t realize that maybe that [EI referral] was something I should definitely do.“ Not evaluated 12 Parents Want to Be Heard • Expertise regarding child • Deciding whether child needs EI 13 Parents as Experts and Decision-Makers “I spend all my time with her, so I know her habits and I know her speech.” Not evaluated “I thought it was my choice, it was my responsibility… to contact [EI] if I felt that he needed services or not.” Evaluated 14 Many families referred to EI did not agree that there was a developmental concern Not Evaluated (n=22) Denial or disagreement Evaluated (n=22) Denial or disagreement 18.2% 63.6% 15 Parental Wait and See • Parents wanted to see if time or working with child at home would help 16 Waiting for Developmental Delay to Resolve or Working with Child “Only if he[’s] getting worse, or he[’s] not improving at all. I will try to talk to somebody to get the situation handled.” Not evaluated “We were like, no, we’ll just work with him, at first. So we tried to work with him. Then at the next appointment he didn’t make too much progress and they were like, yeah we recommend [EI]. So we called the number.” Evaluated 17 Practical Barriers • Time constraints • Not understanding referral process • Contact problems 18 Time Constraints “I did put it in my pile of to-dos, which is a mountain. And it got lost in the mountain.” Not Evaluated “Maybe the child has a lot of appointments. Maybe the child is medically fragile. Maybe mom is overwhelmed. And maybe there’s so many appointments she don’t know which appointment is which. That’s another thing we hear. So sometimes we – we hear that, that’s major. When the child has so many appointments, they don’t understand where we fit and how important [EI] is for their child’s services.” –EI employee 19 Not Understanding the Referral Process "I didn’t have a number to call. I wasn’t really sure why the process was going on and I was also in school. So I just focused on school and didn’t really pay it any mind"- Not evaluated “I feel like I have such short windows of time to spend with my kids that any additional appointments, testing, takes time away. However, if it’s something that’s going to have a remarkable effect or improvement than I would absolutely do it. But time is one, and two just not knowing who to call, where to go.” –Not evaluated 20 Contact Problems “I think she did give me [EI] number too before and I had misplaced it. It seem like every time I got [EI] number I end up misplacing it.” Not evaluated “I did call them and like I said, I think I talked with someone and I think they were supposed to call me back or send me some information or something, but I never heard anything.” – Not evaluated 21 Skepticism • Did parents mistake EI for child protective services and actively avoid evaluation? 22 Child Protective Services “I don’t know about the most difficult. But definitely the most frequent is us being confused with DHS. It doesn’t matter how many times you say it, we’re not DHS.” EI Employee “Some people they already have other issues going on. They might feel insecure about their home environment. It might not look the way other people think it should look. That’s their standard of living. Because it’s in the home, it’s not like you coming to a location, they might feel insecure, like okay I know I’m not the best parent or they might judge me when they come in here, or they might take my kids.” EI Employee 23 Parental Health Literacy Evaluated (n=20) Not evaluated (n=20) Possibly Limited 3 (13.6%) 9 (40.9%) Unlikely Limited 17 (77.3%) 11 (50%) 24 Differences by Health Literacy Level Confusion about EI process Possible limited literacy (n=12) 6 (50 %) Unlikely limited literacy (n=28) 9 (32%) Issues contacting EI 4 (33.3%) 3 (10.7%) Physician does not explain EI 4 (33.3%) 5 (17.8%) No established pediatrician 7 (58.3%) 8 (28.6%) 25 Conclusions • Communication between pediatricians and families often omitted – Straight talk about referral – Practical referral logistics – Listening to families' perception of their child's development, – Addressing parent’s motivation to address concerns. • Impact of parental health literacy on incomplete EI evaluation warrants further study 26