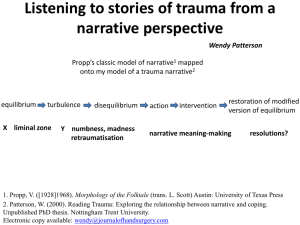
Consequences of trauma
advertisement
The Role of Mental Health following Acute Trauma Elissa J. Brown, Ph.D. Professor of Psychology Director, Child HELP Partnership Scarsdale High School, January 23, 2013 Workshop Outline • Mental health reactions to acute trauma from early to late childhood • Risk factors for post-trauma mental health problems • Immediate, short-term, and long-term interventions • Resources and opportunities for training What is a Traumatic Event? • An experience that is emotionally painful, distressing, and shocking, which can result in lasting physical and/or mental effects. – Actual or threatened death or serious injury – Witnessed or experienced – Response includes intense fear, helplessness, horror • In children, may be disorganization or agitation Characteristics of Traumas • • • • • Acute versus chronic Interpersonal versus non-interpersonal Solitary versus group Perceived as common versus rare Degree and type of impact Consequences of trauma: PTSD A. Traumatic event B. Re-experiencing Intrusive thoughts Nightmares Repetitive play involving the event C. Avoidance/Numbing symptoms Efforts to avoid thoughts, feelings, or conversations Inability to recall important aspect of the trauma Detachment from others Consequences of trauma: PTSD D. Arousal symptoms Difficulty falling or staying asleep Irritability Hypervigilance Exaggerated startle response Psychosomatic symptoms Even if they do not meet full criteria for PTSD, the majority of children report some reexperiencing, avoidance, and/or hyperarousal Consequences of trauma: Differential Diagnosis Attention Deficit/Hyperactivity Disorder Traumatized children may remain motorically active in an effort to keep their minds otherwise occupied Psychosis Need to distinguish between psychotic intrusive thoughts and PTSD re-experiencing. Presence of otherwise intact reality testing in PTSD Trauma-Related Mental Health Problems PTSD and other forms of anxiety Grief and depression Somatic symptoms Risky behavior (alcohol/drug use, self-injury) Aggressive and oppositional behaviors Physical problems (gastrointestinal problems) Attachment and social deficits Academic and learning problems Consequences of trauma: Anxiety Disorders Separation anxiety: fear for loved ones Generalized anxiety: excessive worry Panic attacks Consequences of trauma: Depression • • • • • • • • • Depressed mood most of the day (irritable) Loss of interest or pleasure in activities Significant weight loss (failure to gain weight) Insomnia or hypersomnia nearly every day Psychomotor agitation or retardation Fatigue or loss of energy nearly every day Feelings of worthlessness or guilt Poor concentration Suicidal ideation Consequences of trauma: Behavioral Problems Aggression Oppositional behavior Conduct disorder/juvenile delinquency Toward parents, teachers, and peers In home and school/academic settings Consequences of trauma: Attachment and Social Deficits • Insecure attachments: anger, noncompliance, lack of persistence, little positive affect • Misread social cues • Lower peer status • Fewer social skills • Social networks are more insular and negative Consequences of Trauma Exposure: Academic and Learning Problems • • • • • No overall deficits in cognitive functioning Receptive and expressive language Learning problems Reading ability Comprehension and abstraction Consequences of trauma: In adulthood Major risk factor for: Aggressive and violent behavior Nonviolent criminal behavior PTSD, depression and substance abuse Interpersonal problems Vocational difficulties Medical problems (e.g., cardiovascular) Mental Health Reactions to Traumatic Events • May appear immediately after the trauma or days and even weeks/months later • Reactions of children and adolescents vary according to age, developmental level, and proximity to the event Children’s Reactions to Trauma • Infants and Toddlers (age 3 and under) – Crying – Searching for parents/caregivers – Clinging – Change in sleep and eating habits – Regressive behavior (e.g., thumb sucking, wetting) – Repetitive play or talk Children’s Reactions to Trauma • Preschoolers and Young Children (ages 3-5) – Fear of separating from parents/loved ones – Clinging – Tantrums or irritable outbursts – Sleep disturbance (e.g., wanting parents, nightmares) – Regressive behaviors (e.g., wetting, thumb-sucking) – Withdrawal – Increase in fears (in general: dark, monsters) Children’s Reactions to Trauma • Children ages 6 to 11 years – Regressive behaviors (e.g., school refusal) – Anger and aggression – Avoidance and social withdrawal – Inability to concentrate – Depression and irritability – Fears and worry – Physical complaints (stomach, headaches) – Self-blame Children’s Reactions to Trauma • Adolescents ages 12-17 – Responses may be more similar to adults and specific to the trauma – Depression, guilt/shame, helplessness – General anxiety, panic attacks, dissociation – Numbing, re-experiencing – Mood swings, irritability – School refusal (or academic decline) – Concentration difficulties Children’s Reactions to Trauma • More adolescent symptoms: – Fears: usually event-related (e.g., planes, death) – Anger/resentment – Sleep and appetite changes – Withdrawal (becomes quiet and/or isolates self) from peers, family, teachers, coaches – Physical complaints – Substance abuse Importance of Caregiver Response • Children, particularly young children, tend to be strongly affected by their caregivers’ reactions to the traumatic event • Parents tend to underestimate both the intensity and duration of their children’s stress reactions How long do these reactions last? • Disruptive feelings and behaviors found after an extreme trauma are typical reactions • Need to distinguish immediate phase (hoursweeks after the trauma) from short-term phase (weeks to 2-3 months after the trauma) • There have been few prospective, longitudinal studies of the trajectory of post-trauma mental health problems Children in Decimated Areas: Stress Reactions postHurricane Andrew (La Greca et al., 2005) 35% 30% 25% 20% 3 Months 15% 7 Months 10 Months 10% 5% 0% Moderate Stress Severe Stress Children in Decimated Areas: Stress Reactions postHurricane Andrew (La Greca et al., 2005) • At 3 months, 55% of children with moderate-tosevere distress – 2/3rds of those children were without distress by end of 1-year post-hurricane – 1/3rd of those children (less than 20%) had chronic dysfunction until 10-year post-hurricane • Applying to decimated areas in Queens, we should expect to have 6,600 children continuing to have mental health problems in one year Vulnerability to Post-Disaster Mental Health Problems (e.g., La Greca et al., 2010, in press; Lai et al., 2012) Closer physical and emotional proximity Sense of control, predictability, and safety Exposure to secondary adversities (e.g., displacement) Loss of home, school, community Level of functioning prior to the trauma History of previous traumas Vulnerability to Post-Disaster Mental Health Problems Other stressful life events during recovery period Co-morbid diagnoses Coping style/skills of child and parents Lack of social support of child and family Cognitive processing (e.g., self-blame) High family conflict; low family cohesion Media exposure Summary of Literature (Bonanno et al., 2010) • Disasters cause serious psychological harm in a minority of exposed individuals • Disasters produce multiple patterns of outcome, including resilience • Disaster outcome depends on a combination of risk and resilience factors • The remote effects of a disaster in unexposed populations are generally limited and transient • Disasters put families, neighborhoods, and communities at risk—need to invest now to save later Stages of Intervention • Use research to guide our practice – Immediate/Crisis intervention • Safety and routine are primary • Intervention goal: Educate and normalize – Short-term/Preventive intervention • Identify children and adults at risk • Promote coping and social support – Long-term/Treatment • Treatment of PTSD and other trauma-related symptoms Model of Research/Intervention Trauma Prevention MH Diagnosis Crisis and Preventive Interventions Treatment Prevention • Goals: Prevent emotional and physical trauma • Existing programs – Tend to focus on one form of trauma – Limited research – Poor engagement of participants • Avoidance of topics/trainings • Avoidance of discussion with children Prevention • KEYS: Keeping Every Youth Safe (Brown & Beekman) – Present proven steps for children’s safety • Protecting against sexual abuse • Protecting against excessive physical and verbal discipline – Discuss barriers to taking action – CPR and choking relief – Emergency preparedness • Preliminary research reveals improvements in knowledge and behavior Immediate/Crisis Intervention • Goals: If normal and will heal, why intervene? – Symptoms are painful – Symptoms cause impairment • In child development – Academic functioning – Peer relationships • In adult functioning – Job performance – Friendships and romantic relationships – Parenting • Which, in turn, cause long-term MH problems Research on Crisis Interventions • No randomized trials of hotlines and other forms of crisis intervention • No randomized trials of post-disaster Psychological First Aid or Project Liberty—evidence-informed • Research on Critical Incidence Stress Debriefing – Developed for emergency service personnel – Designed to prevent PTSD – Detailed account of their traumatic experiences • This “debriefing” has been shown to be iatrogenic— associated with higher likelihood of developing PTSD Lessons Learned from 9/11 • Lack of coordination of services/chaos • FEMA funded Project Liberty – Crisis counseling – Provided psychoeducation – Centralized services – Aided with referral • For Hurricane Sandy: Project Hope – Crisis counseling and Psychological First Aid Psychological First Aid—Delivery • • • • • • • • Helpers: Adults on the front-line (paras and profs) Days-weeks after a disaster Be emotionally ready Consider the setting, participants, etc. Maintain a calm presence Be sensitive to culture and diversity Be aware of at-risk populations Be informed of available services Psychological First Aid—Core Actions • • • • Contact and Engagement Safety and Comfort Stabilization (of emotionally overwhelmed) Information Gathering: Current Needs and Concerns – Too early for MH screening—will over-identify number of children who need services (false positives) • • • • Practical Assistance Connection with Social Supports Information on Coping and stress reactions Linkage with Collaborative Services Psychological First Aid: Resources • Outline and materials – http://www.nctsn.org/content/psychological-firstaid • Web-based training – http://learn.nctsn.org/course/category.php?id=11 • App for Iphone – PFA Mobile • In progress: PFA for schools Short-Term/Preventive Intervention • Goals: – Reduce current symptoms – Prevent the development of long-term problems – Identify existing coping skills – Improve functioning – Potentially lower the need for formal mental health treatment – Identify need and refer for treatment if warranted Research on Preventive Interventions • Brief CBT (Psychoeducation and Coping Skills) – Prevented the development of PTSD following a sexual assault (Foa et al., 1995) – More efficacious in preventing anxiety disorders than debriefing or routine community care in children who came through the ED (Silovsky et al., 2004) – 65% less likely than comparison youth to meet criteria for PTSD 3 months post-disclosure of trauma (CFTSI; Marans et al., 2009) Lessons Learned from 9/11 • Continuum-of-care was incomplete – Crisis intervention was available in form of Project Liberty and other services – Evidence-based therapies were available through Child and Adolescent Trauma Services (CATS), NYU Child and Family Recovery Program, and others – There was no preventive intervention Skills for Psychological Recovery: Delivery • After safety, security, and other needs have been met and community is rebuilding • For children and adults – In the short-term – In the long-term who are minimally symptomatic • Minimum of 3-5 sessions; driven by assessment and time since trauma • Helpers: Professionals who provide ongoing support and assistance to children, families and adults (e.g., clergy, educators, librarians) Screening and Assessment Tools • Constructs – PTSD and other mental health problems – Risk and protective factors • Procedures – Structured versus unstructured – Screening versus comprehensive evaluation – Standardized Assessment Instruments • Paper and pencil (e.g., Child PTSD Symptom Scale) • Interview (e.g., UCLA PTSD Reaction Index) • Sources – Child, parent, teacher Skills for Psychological Recovery • Core skills – Building problem-solving skills – Promoting positive and pleasurable activities – Managing physical and emotional reactions to upsetting situations (e.g., triggers, sleep problems) – Promoting helpful thinking – Rebuilding healthy social connections • Done it in Haiti, Puerto Rico—incorporated cultural adaptations Skills for Psychological Recovery: Resources • Information on the National Child Traumatic Stress Network website: – http://www.nctsn.org/nctsn_assets/pdfs/newslett ers/Impact_Summer_2010.pdf • Child HELP Partnership will be providing training and supervision on the model starting in early 2013 Long-Term Solutions • Repeat assessment of trauma-related mental health symptoms and functional impairment • If trauma-related symptoms continue or worsen, access evidence-based, traumainformed therapies – Trauma-Focused Cognitive Behavioral Therapy (TFCBT; Cohen, Mannarino, & Deblinger, 2006) – Cognitive Behavioral Intervention for Trauma in Schools (CBITS; Jaycox, 2003) Treatment Research • TF-CBT and CBITS are the most rigorously tested treatments for traumatized children • More than 12 randomized trials – Improved PTSD, depression, anxiety, and behavior problems compared to supportive treatments – TF-CBT improved parental distress, parental support, and parental depression compared to supportive treatment – Effective in individual/family and group formats – Symptom decreases maintained at 2-year follow-up – Findings replicated and generalized across racial, ethnic, and geographic boundaries (King et al., 2000) Lessons Learned from Hurricane Katrina • Field trial of TF-CBT and CBITS (Jaycox et al., 2010) • Assessment 15 months after the hurricane • 60.5% of children screened positive for PTSD and were offered CBITS at school or TF-CBT at a mental health clinic • Both lead to significant symptom reduction • More children chose CBITS • Greater symptom reduction for TF-CBT Difficulties Addressed by TF-CBT • CRAFTS Cognitive Problems Relationship Problems Affective Problems Family Problems Traumatic Behavior Problems Somatic Problems Core Values of TF-CBT • CRAFTS Components-Based Respectful of Cultural Values Adaptable and Flexible Family Focused Therapeutic Relationship is Central Self-Efficacy is emphasized TF-CBT Components • PRACTICE Psychoeducation and Parenting Skills Relaxation Affective Modulation Cognitive Processing Trauma Narrative In Vivo Desensitization Conjoint parent-child sessions Enhancing safety and social skills TF-CBT Sessions Flow Baseline Assessment Entire Process is Gradual Exposure Sessions 1-4 Psychoeducation Parenting Skills 5-8 Trauma Narrative Development and Processing Relaxation Affective Expression and Regulation Cognitive Coping In-vivo Gradual Exposure 9-12 Conjoint Parent Child Sessions Enhancing Safety and Future Development TF-CBT: Child and Parent Components • Individual sessions for both child and parent • Parent sessions - generally parallel child sessions • Same therapist for both child and parent A Learning Resource for TF-CBT Access at: www.musc.edu/tfcbt •Web-based learning •Learn at own pace •Concise explanations •Video demonstrations •Clinical scripts •Cultural considerations •Clinical Challenges •Resources •Links •10 hours of CE •Free of charge Structure of CBITS • School-based intervention –10 week groups –1 class period/week –Individual sessions for trauma narrative –6-8 children per group –Run by a clinician Difficulties Addressed by CBITS • Reduce symptoms of: – PTSD – Depression – Behavioral problems • Improve: – Functioning – Grades and attendance – Peer and parent support – Coping skills CBITS Components • • • • • • • • Psychoeducation Relaxation Social problem solving Cognitive restructuring Exposure Between Homework assignments and activities 2 parent and 1 teacher education sessions CBITS Resources • Developer: Lisa Jaycox, PhD, Rand Corporation • Website: – http://cbitsprogram.org/ • Audra Langley, PhD Director of Training – alangley@mednet.ucla.edu Taking Care of the Care Takers • Protect against your own secondary stress / vicarious trauma response: – Use your colleagues/supervision to process your own feelings and experiences – Engage in self-care • • • • Basics: eating, sleeping Exercise Social support Coping skills Resources • Resources for Traumatized Children and their Caregivers – National Child Traumatic Stress Network http://nctsn.org/trauma-types/natural-disasters – TF-CBT web www.musc.edu/tf-cbt • Resources for Adults – National Center for PTSD http://www.ptsd.va.gov/ – International Society for Traumatic Stress Studies http://www.istss.org/Home.htm Resources • Mental Health Support and Services in Your Area – Disaster Distress Helpline 1-800-985-5990; text 'TalkWithUs' to 66746 (Spanish-speakers can text 'Hablanos' to 66746) – LIFENET • 1-800-LIFENET; 1-877-AYUDESE (for Spanish speakers) • 1-877-990-8585 (for Korean and Mandarin and Cantonese speakers) – Health Information Tool for Empowerment (HITE) • www.hitesite.org Resources • Mental Health Support and Services in Your Area – The Child HELP Partnership • 718-990-2367 • www.stjohns.edu/thechildhelppartnership • browne@stjohns.edu • Developers/trainers of Keeping Every Youth Safe • Trainers in Skills for Psychological Recovery • Trainers in trauma-specific therapies