Transition in Epilepsy Services - The Association for Young People`s
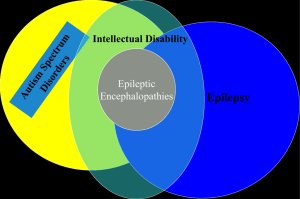
advertisement
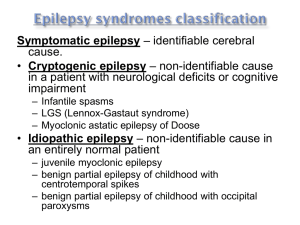
Transition in Epilepsy The Transition of Patients with Epilepsy from Paediatric to Adult Care Services across the Aneurin Bevan Health Board Kostov, C., Lewis, H., Syed, N., Lawthom, C., James, L., Capeling, L., SpenderThomas, K., Barber, M. Personal Reasons for Interest in Audit Paediatrics Personal experience of difficulties of falling between paediatric and adult care Similar age to those transitioning Background - Epilepsy • Newly emerging sub-specialism • Paediatricians developing specialist interest • Transition is recognized as an area for improvement in the care of young people with epilepsy1,2 • Joint clinics are emerging as a way of facilitating the transfer to adult care • First teenage epilepsy clinic – Liverpool 1991 • University Hospital of Wales, Cardiff - 1996 (17 years) Specialist Tertiary Teenage Clinic • ABHB – past 18 months http://www.wales.nhs.uk/nhswalesaboutus/structure10 An Action Plan following the results of the ‘Epilepsy12’ National Audit suggested that ABHB: “establish a transition care pathway and to formalize handover clinics” 3 Objectives for Audit 1. Current Practice 2. Professionals’ perspectives 3. Views of patients and parents/carers Case ascertainment Records of notes of patients discharged from Paediatric Epilepsy Specialist Nurse services Learning Disability Transition Database Consultant-led & Nurse-led Transition Clinic Lists What we did: 1. Case Notes Review 1. Questionnaire to professionals 2. Questionnaire to patients and parents/carers Results 19/34 (56%) of patients had learning disabilities 22/34 (62%) had other co-morbidities (Cerebral Palsy, Autism, Sensory impairment) 24/34 patients were referred: 7/24 (29%) of referrals made requested advice regarding diagnosis, investigations and medication Only 13/24 (54%) referrals made based on age alone First Appointments in Adult setting: 16/22 (73%) patients attended a joint clinic: 17/22 (77%) had additional problems recorded 15/22 (68%) had medications altered Only 3 patients had transitional planning meetings recorded 2 attended by educational / social workers Only 2 patients had a transition coordinator documented (62% had co-morbidities) What did Professionals Think? 73% of Paediatric Professionals rated current transition as ‘Poor’ Confusion regarding Referral Pathways… 1. All to Adult Neurologist (A) Based on complexity and control of epilepsy: (B) Based on learning disabilities: 2. Complex epilepsy to teenage clinic UHW, all others to adult neurologist 4. Learning disability to Learning Disability/Psychiatry services and LD nurse, all others to GP 3. Complex to adult neurologist, well controlled to GP (C) Based on complexity/control of epilepsy & whether additional learning disabilities: 5. Learning disabilities to Psychiatrist, complex epilepsy to adult neurologist, all others to GP. 10/11 (91%) of paediatric professionals felt a transition proforma would be helpful… Collaborative working between professionals: Only 4/8 (50%) of consultant paediatricians felt they work closely with adult neurologists, and vice-versa 3/6 (50%). 4/9 adult and 4/11 paediatricians ran transition clinics At handover, adult specialists wanted to know about medication history, diagnostic work-up and lifestyle Information provided “incomplete” and “variable” 8/20 (40%) professionals had received training in transition 14/20 were aware of transition policies – only 3 felt able to adhere to them Views of Professionals Main areas for improvement: “Explicit transition care pathway” “Better coordinated approach between Paeds and Adult Neurology and Learning disability services, and health, education and social services” Views of Professionals… “Current practice variable with no uniformity in provision of transition services” “It is crucial that ABHB recognize and support both paediatric and adult epilepsy services in the implementation of transition services/care” What did Patients and Parents Think? 45% of patients and parents/carers found transition ‘difficult’ or ‘very difficult’ Some patients reported a “very traumatic experience” and found it “difficult to cope with change” Several thought the process should have started much sooner 6/11 (55%) attended joint clinics: 5 patients thought they were helpful One parent reported the “first appointment was useful then it drastically fell apart” Did patients and parents/carers feel they received enough information? 6/11 (55%) of patients felt supported throughout their transition 5/11 (45%) felt in control of the process Young people’s views: “ I don’t think anyone feels in control as healthcare worker ‘knows best’ ” “ I wanted better understanding and to be treated as an individual ” Views of Patients and Parents / Carers Difficulties faced in Adult Care: “Confusion regarding person responsible for providing/updating epilepsy care plan” “All therapies..severely curtained leaving [young person] more isolated and less likely to achieve any goals” Views of Patients and Parents/Carers… “Transition should start at 14 when multiple problems with at least two appointments with consultants from paediatrics and adults so that all information is handed over properly” “Information needs to be made more readily available..I did feel somewhat ‘in the dark’ ” “My paediatrician came to my first meeting with the neurologist. This was helpful and ensured a seamless transition” http://www.bigstockphoto.com/image-6644085/stock-vector-two-cartoon-doctors Discussion Transition is difficult for patients with epilepsy Joint clinics are deemed successful by patients and professionals Transition overall is still rated poorly Key elements for good transition: • Patient centered transition plan • All professionals working together towards a joint goal • Training of professionals • Resources A process, spanning the teenage years. What is needed? Care pathways to be refined Clarification of referral pathways Roles and responsibilities of professionals involved in transition clearly defined Access to joint clinics Efficient transfer of information Limitations Case ascertainment – lack of database Retrospective analysis Risk of bias with questionnaires Conclusion • Good elements emerging • Scope for improvement and formalisation of care pathways – clarification; promote equality of care • Proforma • Consider views of: Patients and parents/carers Professionals in primary health Paediatricians and Adult neurologists Learning disability services ..In medical and specialist nursing professions. • Care pathways to be refined locally, • collaborating widely • specific needs of each patient - control of epilepsy, extent of comorbidities, professionals involved in their care. ABHB are currently developing an electronic database - highlight patients approaching 14 years Personal Reflections Difficulties of an Audit! Qualitative Data Working between paediatric and adult teams Patients and parents forthcoming and grateful for giving feedback Huge amount of willingness and motivation for improvements Thank you. Any Questions? References References 1. National Institute for Clinical Excellence (NICE). (2012). The Epilepsies: Diagnosis and Management of the Epilepsies in Adults and Children in Primary and Secondary Care. Available at: http://www.nice.org.uk/nicemedia/live/13635/57779/57779.pdf. 2. Department of Health (DH). (2008). Transition: Moving on Well. Available at: http://www.bacdis.org.uk/policy/documents/transition_moving-on-well.pdf. 3. Epilepsy12 Audit – Action Planning 2012. (2012). Gwent Action Plan. Available at: http://www.rcpch.ac.uk/system/files/protected/page/Gwent.pdf. 4. Aneurin Bevan Health Board. (2012). Policy for Transition of the Young Person with Healthcare needs between Children’s Services and Adult Services within the Aneurin Bevan Health Board. 5. http://www.wales.nhs.uk/sitesplus/866/home