Anatomy, Function of Human Skin
and Diagnosis
Dr . Ali elethawi
Specialist dermatologist
C.A.B.D ,F .I .C.M.S
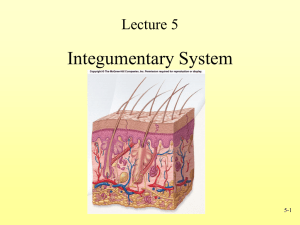
• The integumentary system is synonymous with:
The skin and its appendages :
sweat glands, nails, hair, sebaceous glands & arrector pili muscles.
Mammary glands
Teeth
The skin:
is the interface (surface) between human & environment
largest organ in the body:
• 16% of our body weight ≈ 4kg
• Its surface area is of 1.8 - 2 m2
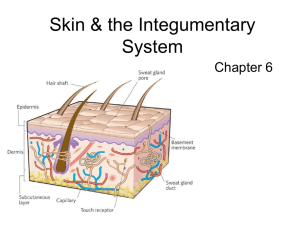
skin layers:
Skin has three layers:
1.The epidermis, the outermost layer of skin,
provides a waterproof barrier and creates our
skin tone.
2.The dermis; beneath the epidermis, major structural element
• Three types of components (cellular, fibrous matrix, diffuse and
filamentous matrix).
• Also site of vascular ,lymphatic, and nerve networks.
3.The subcutaneous tissue (hypodermis):
is made of fat and connective tissue.
Normal Skin
Normal Skin Low Power with Labels
skin can be classified as thick or thin:
1) Thick skin
- covers palms and soles,
- has sweat glands, but lacks hair follicles, arrector pili
muscles, and sebaceous glands
2) Thin skin
- covers most of the rest of the body
- contains sweat glands & hair follicles, arrector pili
muscles, and sebaceous glands.
skin can also be classified as hairy &non hairy
1.Non hairy skin: Lip, glans penis, labia minora, palms,
soles
2.hairy skin : covers most of the rest of the body
Epidermis:
It is stratifed squamous epithelium
epithelium thickness vary from 0.05mm in eyelids to
1.8 mm in palm & sole
upper layers dead, filled with keratin (waxy protein)
lower layers living cells
avascular( No blood vessels)
replaced every 35-45 days (i.e: Transit time: is the
time needed for cell maturation from basal layer to
the surface, normally = 35-45 days)
Layers of epidermis
1. Basal layer ( stratum basalis):
•
•
•
•
•
•
•
single layer of columnar cells
deepest layer,
Actively dividing cells : In normal skin 30% of basal cells are preparing
for division (growth fraction)
only cells that get adequate nutrition and oxygen by diffusion from tissues below
bordered below by basement membrane : hemidesmosomes attached
them to underlying lamina densa of BMZ
2. Spinous (prickle) cell layer:
7-9 layers of cells
keratinocytes larger than basal layer.
Keratinocytes firmly attached by
cytoplasmic process (desmosomes) &intercellular
glycoprotein cement
Tonofilaments are small fibers running from cytoplasm to
desmosomes
3. Granular layer:
• 2-3 layers
• Contain irregular basophilic granules of keratohyalin .
• Cells flatter than spinous layer,
• No nucleus
• No intracytoplasmic organelles
• More tonofibrils
• as cells move up from s. basale they die & get flatter
and thinner
• keratinization begins here
4. Stratum Luidum:
Thin translucent band.
Only in palms & soles
5. Stratum corneum: SC:
Made of many layers of flattened dead cells (corneocytes),
•
has no nuclei or cytoplasmic organelles.
• like Bricks-stuck together by intercellular lipids
• water resistant
Cells of epidermis
1. keratinocytes : most (80%) cells in epidermis synthesize
keratin
2. melanocytes : found in the deepest layer synthesize melanin
pigment.
3. Merkel cells : touch receptors, attached to nerve cell
4. dentritic cells(Langerhans cells) : found in st. spinosum
and st. granulosum are : if detected antigen they alert immune
system (antigen presenting cell)
5.stem cells : undifferentiated cells found only in deepest layer
basement membrane zone
the basement membrane lies between epidermis & dermis
Composed of:
• Hemidesmosomes of the basal layer ; attach to lamina densa of BMZ
• Lamina Lucida: is electron lucent area lies below basal cell layer.
• Lamina Densa : Fine anchoring filaments cross lamina lucida & connect
lamina densa of plasma membrane of basal cell layer.
• Anchoring fibrils, :extend from
deep part of lamina densa to papillary dermis
Function :
1. Provide mechanical support
2. Encouraging adhesion, growth, differentiation & migration of overlying
basal cells
3. Act as semipermeable filter that regulate transfer of nutrients & cells
between dermis & epidermis
Dermis:
gel-like matrix Lies between epidermis & subcut. Fat
strong, flexible, connective tissue gives skin its strength and resilience
Support epidermis structurally & nutritionally
It contain cells ,fiber , ground substance, nerves endings, muscles, skin appendages ,
lymphatic vessels and blood vessels .
LAYERS OF DERMIS; structurally divided into two areas:
1. Papillary layer : a superficial thin area adjacent to the epidermis,. mainly areolar
connective tissue , dermal papillae (capillary loops ,sensory cells)
2. reticular layer :a deep thicker area. mainly dense (irregular connective tissue)
dermal tearing = stretch marks.
Dermis Interdigitate with epidermis.
Dermal papillae is upward projection of dermis
Rete ridges: is the downward ridges of epidermis
This allow adhesion between dermis & epidermis as it increases the surface area between
them
Cells of dermis
The dermis is composed of three major types of
cells:
• Fibroblasts.
• Macrophages.
• Adipocytes.
fibers of dermis
Collagen fibers:
• make 70-80% of dermis dry weight
• Compose of thinner fibrils packed in bundles
• Made of 3 polypeptide chains; (proline, hydroxyproline, glycin)
• Its tensile strength prevent tearing when skin is stretched.
Elastic fibers:
2% of dermis dry weight
elastin is made up of polypeptides rich in glycine, desmosine,
valine
Have amorphous elastin core surrounded by elastic tissue
micrifibrillar component
Reticular fibers: fine collagen fiber found in fetal skin , adult skin
appendages& around bl.v.
Ground substance of dermis
Composed of
glycosaminoglycan (hyaluronic acid & dermatan sulphate)
with smaller amount of heparan sulphate & chondroitin
sulphate
Functions:
allowing nutrients, hormones & waste
products to pass through dermis
Acts as lubricants between fibers
Provides bulk act as shock absorber
Muscles
Smooth arrector pili muscle
1- sebum expression
2- goose pimples from cold,
3- nipple erection
smooth dartos muscle ;raising of scrotum
Striated fibers (platysma) & some of muscles
of facial expression found in dermis
Blood vessels
• 2 main horizontal plexus, superficial & deep
• Under sympathetic nervous control .
• Regulate body temperature
Nerves
• One million nerve fibers mostly in the face &
extremities
• Both mylinated & unmyelinated fibers exist
• Itch is follow stimulation of free nerve endings
close to dermo-epidermal junction
Hypodermis( subcutaneous tissue).
lies below the dermis.
attach the skin to underlying bone and muscle
as well as supplying it with blood vessels and nerves.
• It consists of loose connective tissue and elastin.
• The cells are: adipocytes (main cell ;the hypodermis
contains 50% of body fat) ,fibroblasts& macrophages
Fat serves as padding and insulation for the body.
The Physiology of Skin
• The skin is a metabolically active organ with
vital functions such as protection and
homeostasis.
Functions of the skin
1.Provides a protective barrier against mechanical,
thermal and physical injury and noxious agents.
2.Prevents loss of moisture.
3. UV protection Reduces the harmful effects of UV
radiation.
4.Acts as a sensory organ.
5. Thermoregulation ,helps regulate temperature
control.
6.Plays a role in immunological surveillance.
7. Synthesizes vitamin D3 (cholecalciferol).
8.Has cosmetic, social and sexual associations.
Skin appendages (Adnexa):
1. Sweat glands
2. Hair
3. Arrector pilli muscle
4. Nails
5. Sebaceous glands
Sweat Glands
Eccrine glands Sweat Glands
• ~3 Million total on skin, ~3000 sweat glands/inch2
• most numerous on palms, soles, forehead, armpits
• essentially a tiny coiled tube that opens to skin surface
• secret sweat ; helps maintain temperature and fluid/electrolyte balance
• stimulated by heat ----- ‡ sweat ‡ evaporative cooling
Apocrine sweat glands
• much less common, modified sweat glands
• confined to axillary and genital area
• their ducts open into hair follicles
• secretions contain fatty acids and proteins in addition to “sweat”
• respond especially to stress and sexual stimulation
Skin Glands
Sebaceous Glands( Oil glands , holocrine)
2 or more per hair follicle
secrete sebum = breakdown products of dead cells.
keeps hair soft and pliable esp. on face and scalp
Not found on palms, soles or dorsal side of feet
reduces heat loss
lipids are poor heat conductors ----helps prevent water
evaporation
become active at puberty ‡ acne
Mammary Glands
modified sweat glands
produce milk
Ceruminous Glands
modified sweat glands
in external ear canal
secrete waxy pigmented cerumin
protection , traps dust and particles
Hair
• the hair on the scalp does protect us from UV radiation
and minor injury.
• But today, the hair is of cosmetic value.
Hair follicle form before nine week of fetal life when hair
germ grows obliquely down into dermis.
Types of hair: 1- Lanugo hair 2- Vellus hair 3- Terminal
hair
Hair growth (Hair cycle) is cyclical and has 3 phases:
anagen, catagen & telogen
Nails
• Hard keratin of nail plate formed in nail
matrix which lies in an invagination of
epidermis on back of terminal phalanx of
digits toes
• It provide strength & protection for terminal
phalanx & allow handling of fine objects
• Finger nail growth is 0.5-1.2 mm per week
• Slower in toe nails
• Faster growth in summer
Skin Embryology:
Origins of the Integumentary System: (The Skin)
The epidermis is from surface ectoderm.
• The dermis is derived from mesoderm.
Hair: A hair follicle develops as a proliferation of the epidermal
stratum germinativum and extends into the underlying
mesenchyme.
Nails: develop from thickened areas of epidermis at the tips of each
digit called nail fields.
• Later these nail fields migrate onto the dorsal surface surrounded
laterally and proximally by folds of epidermis called nail folds
• Both the sebaceous glands and sweat glands
( mammary glands) are derived from the epidermis and
grow downwards into the dermis.
• The majority of sebaceous glands originate as buds from developing
hair follicle root sheath.
• Sebaceous glands in the glans penis and labia
minora (independent of hair follicles) develop
similarly, but as buds from the epidermis.
1- Primary Lesions( basic): are the first to appear
and are due to the disease or abnormal state.
• Must be distinguished from secondary or
induced lesions
Macule-patches
Papule- Plaque
Nodule- Tumor
Purpura -Petechiae –Ecchymosis- Haematoma
Wheal
Vesicle-bulla
Cyst
Pustule- abscess
Infarct
Telangiectasia, Erythema, Angiodema, Burrow, Comedo & Poikiloderma
Macule (Latin: macula, “spot”) < 5mm
is a circumscribed area of change in skin color without elevation or depression
Macule < 5mm
patches > 5mm
Erythema: is redness caused by vascular dilatation
Papule: is a superficial, elevated, solid lesion, generally <0.5 cm in diameter
Plaque A solid lesion more than 0.5 cm in diameter,
often formed by the confluence is a plateau-like elevation above
the skin surface
Nodule
A circumscribed, elevated, solid lesion, Larger than papules: > 5 mm diameter (in
both depth & width)
tumor :Large nodule
Vesicle-Bulla ( Blister ) is a circumscribed elevated, superficial cavity containing
fluid
A vesicle <0.5 cm
A bulla >0.5 cm
pustule
is a circumscribed, superficial cavity of the skin that contains a purulent exudate
Abscess: localized collection of puss more than
1 cm in diameter
Wheal: elevated, transitory, compressible papule or plaque produced by dermal
edema
Angiodema: is diffuse swelling caused by
subcutaneous oedema
Cyst: an epithelial lined cavity containing liquid or semisolid material (fluid, cells,
and cell products)
Petechiae: pinhead sized macules of blood
Purpura: larger macule or papule of blood
Ecchymosis: a collection of blood greater than 1
cm in size outside the vascular tree
(extravasation of blood), in the skin and within
tissue
Haematoma: is swelling from gross bleeding
Burrow: is linear or curvilinear papule as in
scabies
Comedone : is a plug of greasy keratin wedged in
a dilated pilosebaceous orifice
2- Secondary Lesions:
From the natural evolution of primary lesions
-
•
•
•
•
•
•
•
•
•
•
•
scale,
ulcer,
crust
erosion
excoriation
lichenification,
atrophy
scar
fissure,
Sinus,
Keratosis& Striae
scar
Scar: is a pattern of healing where normal structures replaced by fibrous CT at a
site of injury to the dermis
1- Hypertrophic or
2- atrophic scar.
3- Sclerotic or hard Scar
atrophy
Atrophy: Thinning of skin caused by diminution of epidermis, dermis or subcut.
tissue
Ulcer: a "hole in the skin"
• circumscribed area of skin loss extending through the
epidermis and at papillary dermis heals with scarring
Erosion
Erosion: moist, circumscribed, usually depressed lesion due to loss of
all or part of the epidermis, heals without scar
Crust: scab :A collection of dried serum and cellular debris
Excoriation:
• Epidermal linear or punctate
• superficial excavations (ulcer or erosion)
• caused by scratching, rubbing, or picking.
Lichenification: chronic thickening of the skin
along with increased skin markings.
• Results from scratching or rubbing
Fissure: is a skin slit
• Heel fissure
Sinus: is a cavity or channel permits escape of
fluid or pus
Keratosis:
is a horn like thickening of stratum corneum(SC)
Striae: ( stretch marks).
is a streak like linear atrophic pink purple or
white lesions..