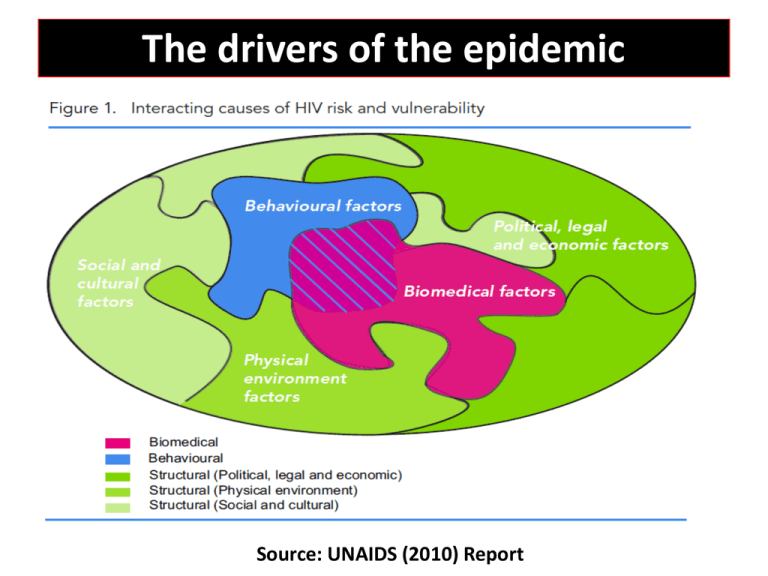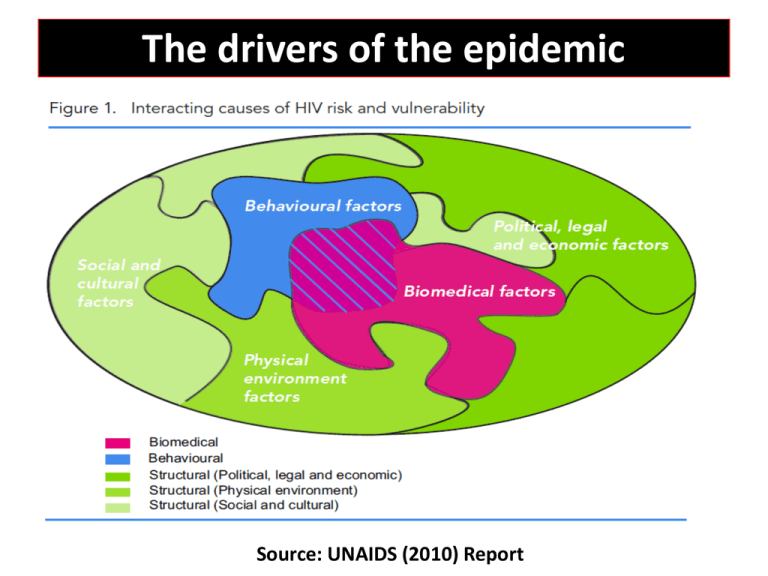
The drivers of the epidemic
Source: UNAIDS (2010) Report
Combining
Social, Behavioral & Biomedical Science
in
Prevention of HIV
Noah Kiwanuka, MD,PhD
Makerere University College of Health Sciences
School of Public Health
Prevention: an urgent global priority
Despite declining HIV incidence globally, for every individual started on
ART, 2 new HIV infections occur. Thus strengthening HIV prevention
remains an urgent global health priority (UNIADS report, 2010)
To-date, a number of HIV prevention interventions can significantly
reduce new infections with varying degrees of efficacy (31 – 96%).
These include among others:
Biomedical
-
ART for infected (PEP and Rx for prevention),
ART for uninfected but exposed persons (PREP, microbicides)
Safe male circumcision
Prevention of mother-to-child transmission
Socio-behavioral
- Consistent condom use,
- HIV testing and counseling, behavioral change,
Combination prevention
• Since none of these interventions can singly eliminate HIV, it is
plausible that when used in combination with each other, they
can dramatically reduce or possibly eliminate new HIV infections.
• UNAIDS (2010) definition of combination HIV prevention
“The strategic, simultaneous use of different classes of
prevention activities (biomedical, behavioral, social/structural)
that operate on multiple levels (individual, relationship,
community, societal), to respond to the specific needs of
particular audiences and modes of HIV transmission, and to
make efficient use of resources through prioritizing,
partnership, and engagement of affected communities”
Combination prevention- 2
– Evidence informed strategic, and simultaneous use of
different complementary behavioral, biomedical and
structural interventions
– to address both the immediate risks and underlying
causes of vulnerability to HIV infection, and the
pathways that link them,
– so as to generate significant and sustained reductions
in HIV incidence in diverse settings.
[Hankins CA, and de Zalduondo BO, AIDS. 2010 Oct;24 Suppl 4:S70-80].
Role of different disciplines to
HIV combination prevention
science
Epidemiology
• Identify key populations at risk
– CSWs, Fisher folk, MSM, IDUs
• Determine risk factors and magnitude of risk
– Prevalence, incidence, attributable risk
• Evaluation of impact of interventions – single or
combination
– Efficacy
– Effectiveness (individual and population)
Social Sciences
• Identify and determine characteristics of risk
behaviors and change/modification
– Sexual networks and mixing
• Understand modes of and reasons for various risky
behaviors
– Multiple partners, unprotected sex, unfaithfulness
• Understand issues of demand generation for
combination prevention
– High risk folks not coming for SMC, why?
– Eligible persons coming late for ART
– Poor adherence to ART
Basic Sciences
• Biology of HIV and immune response to infection
– What HIV is, how is infect human cells, and its interaction with the immune
system, and causes disease,
– Different types and subtypes and their implication to natural history
– Why host immune response doe not fully control HIV infection?
– How reservoirs of infection persist in body despite HAART?
– Correlates of immune protection etc
• Biological basis of risk, infection, and protection
– Biological endpoints and biomarkers
• infection, progression, response
– correlates of risk and protection
Ideal combination prevention package (s)
• Evidence-based,
• Complementary,
• Feasible / appropriate,
• Applicable /deliverable (high level of coverage)
• Acceptable (with high adherence),
• Efficacious and effective (individual & population)
• Cost-effective
• Sustainable
Challenges
Which of proven individual interventions can be combined?
Criteria for inclusion of an intervention in a prevention “package?”
–
–
–
–
–
Magnitude of impact
Nature of studies adducing evidence? RCTs, observational
Number of studies (in various population settings)
Consistency of results
Examples
• High impact on HIV incidence, multiple RCTs—PMTCT , MMC,
• High impact on HIV incidence, single RCT—PREP HPTN052.
• Moderate impact – Microbicides CAPRISSA 004 , iPREX,
• Evidence based on preliminary data, observational data, plausibility of
intervention ( faithfulness, consistent condoms use, STI Rx, preventive
HIV vaccine.
Challenges - 2
No evidence yet on efficacy/effectiveness of combination
prevention – current evidence based mainly on single
interventions
– On-going studies in Botswana, South Africa
Interventions found to be efficacious in one setting may not
necessarily be replicable in other settings and may require
cultural adaptation.
Impact of combination prevention on health systems and nonHIV services
Challenges -3
• Sexual networks and intra- and intercommunity transmission.
Rakai, spatial clustering statistics, phylogenetic analyses, and
probabilistic transmission models
- 43% of transmissions occur within stable household partnerships,
- Of those who acquire HIV infection from extra-household sexual contacts
are more often infected by partners from outside (63%) than from within
their community (37%).
What are the implications on locally targeted “test and treat”