A Method for Evaluating Personal Protective Equipment Technique
advertisement
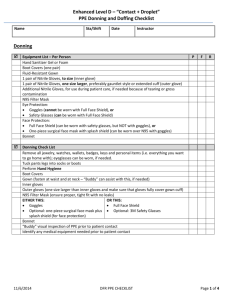
Elizabeth Beam, RN, MSN UNMC College of Nursing Special thanks to Dr. Gibbs, Kate Boulter, Marcia Beckerdite, and Dr. Philip Smith MD The plan Key concepts in PPE for healthcare. Describe study. Results and discussion. Future directions. Questions? If time…video review simulation. Key concepts in personal protection for healthcare… Proper order for donning PPE What PPE to wear Contact Contact & Droplet Contact & Airborne How to protect yourself while in the patient room Proper order for doffing PPE A pilot study… A study was conducted to examine the feasibility of employing a simulated healthcare environment to assess the technique of healthcare workers in the use of standard airborne and contact isolation precautions without the potential for harm to real patients. Powdered fluorescent marker tracking and digital video recording were used to assess compliance with current guidelines. An expanded research study will be needed to further examine these commonly noted contamination and exposure pathways. Simulation suite… Faking it… Glowing germs… Guidelines… Centers for Disease Control http://www.cdc.gov/HAI/prevent/ppe.html World Health Organization http://www.who.int/csr/resources/publication s/WHO_CDS_HSE_2008_2/en/index.html Scenarios… Registered Nurses hung an intravenous (IV) medication (IV line into bag under gown) and performed a head-to-toe assessment on the patient. Respiratory Therapists assessed the patient and administered a nebulizer treatment (saline only). Nursing Technicians repositioned the patient from bed to chair, took vital signs, and conducted input and output assessment. Poster used in study… Color copies Posted at donning and doffing areas. Summary of study design… Simulation Room Cameras (in room, outside room) Simulated Patient (yours truly) Glo Germ Job-specific procedures (simulated) Nurse: IV med RT: Nebulizer treatment Patient care tech: Reposition, I & 0, VS Randomized: Guideline poster available Participants: Healthcare workers (n=10) Convenience sample Good skill mix (med-surg, ICU, ER, etc.) Had experience with simulation Multiple genders, roles, etc. Video Results… Each of the 10 participants committed at least one breach of standard airborne and contact isolation precautions Donning: Most common: not conducting a seal check on the respirator, failing to tie the gown at both the neck and the waist, and improper sequence. Doffing: Most common: improper sequence, the method for removing the respirator, and removing potentially contaminated items from the room. In room: Touching self with dirty gloves. Touching surfaces in room for no apparent reason. Glo germ results… Glo Germ noted with UV light and digital photographs taken: Contamination noted in 8 of the 10 participants. 6 hand area; 3 back of head. One had contamination on both their hands and their head. Discussion… Our study was not large enough to determine if poster impacted behavior, but… Is it Glo Germ or is it paper towel debris? Video capture: Good quality. Interesting data. Camera position matters. Simulation lab vs. regular hospital room with mounted digital cameras? Dissemination… Beam, E., Gibbs, S., Boulter, K., Beckerdite, M., & Smith, P. (2011). A method for evaluating personal protective equipment technique by healthcare workers. American Journal of Infection Control, 39, 415-420. Future directions… “Body of Work” creates questions: What are the common errors? Are there facility-specific errors? Do physical characteristics matter? Why are the poor behaviors seen? What are the beliefs among healthcare workers about PPE? Could reflective practice improve performance? Mixed Methods Study Investigating Infection Control Behavior Population: Registered Nurses expected to care for patients in isolation in the hospital. Sample Size: Minimum 30. Pre-simulation data: Collect demographic information, occupational history, and physical characteristics/flexibility assessment. Simulation Experience: Video Record Patient Care + Review video with ‘Think Aloud’ Recording Sequential Explanatory Design: Simulation will be reviewed and scored (as per Beam, et al., 2011). Think Aloud recordings will be qualitatively analyzed (Max QDA). Long Term Follow Up (at One Month): Interview asking about change in practice.