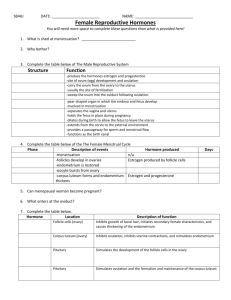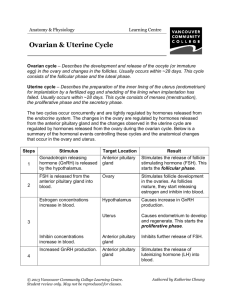
C) The Menstrual Cycle
•The female menstrual cycle takes an
average of 28 days. (Variation is
common).
•The cycle occurs in four phases if no
fertilization occurs:
1.
are
Menstrual Phase
(Day 1-5)
i)
Thick
endometrium tissues
shed from the
mucosa of the
uterus.
ii)
Produces
menstrual flow.
2.
Follicular Phase (Day 6-13)
The hypothalamus
stimulates the pituitary to
release FSH which causes
a follicle containing an
ovum to develop.
One follicle develops the
fastest & this follicle
secretes estrogen which is
responsible for female
secondary sex
characteristics.
Female secondary sex characteristics:
- development of breasts & body hair
- increased thickening of the endometrium
Increased estrogen levels also stimulate
the release of LH from pituitary. This
triggers ovulation.
LH levels rise near day 14.
The follicle migrates to the surface of the
ovary.
3)
Ovulation - Day 14
Dominant follicle
pushes on the
outer wall of
ovary. The outer
wall of the ovary
bursts and the
ovum is released
from ruptured
follicle.
The ovum is picked up by fimbrae which
sweep ovum into fallopian tube.
Follicular cells (from ruptured follicle),
differentiate into the corpus luteum.
Accompanied by a brief rise in body temp.
Follicular Phase
Ovulation
Luteal Phase
4)
Luteal Phase (Day 15-28)
Marked by
development of
corpus luteum
Estrogen levels
decreased when
the oocyte left the
ovary but are
restored
somewhat when
the corpus luteum
forms.
Corpus luteum secretes both:
estrogen and progesterone.
- Further thickens & maintains the
endometrium.
- inhibits further ovulation – why birth
control pills contain high amounts of
progesterone.
- prevents uterine contractions.
If fertilization does not occur, the
corpus luteum disintegrates into a scar
called the corpus albicans.
The concentrations of estrogen &
progesterone decrease, thereby causing weak
uterine contractions. These contractions cause
the endometrium to pull away from the uterine
wall. This marks the beginning of the flow
phase.
If fertilization has occurred, the corpus
luteum remains in order to keep estrogen &
progesterone levels high until the placenta
forms.
Menstruation begins as endometrium is
lost due to lack of estrogen and
progesterone.
Hormonal Control of the Female
Reproductive System
-dev. of breasts
& body hair
- increased
thickening of
endometrium
-Prepares
uterus for
embryo by
stimulating
endometrium
- inhibits
further
ovulation.
- prevents
uterine
contractions.
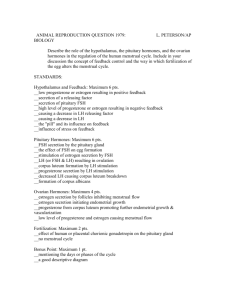
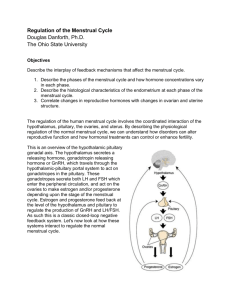
The production of estrogen and progesterone
(hormones of the ovary) is regulated by the
hypothalamus-pituitary complex.
Gonadotropins (female FSH and LH) regulate
the control of hormones produced by the ovary.
The onset of female puberty causes the release
of GnRH (gonadotropin releasing hormone)
from the hypothalamus. GnRH stimulates the
anterior pituitary to release FSH and LH, which
are then directed to the ovaries.
Follicular phase:
During the follicular phase of the
menstrual cycle, FSH secretions are carried
by the blood to the ovary, where follicle
development is stimulated.
The follicles secrete estrogen, which
stimulates the development of secondary
sexual characteristics and initiates the
development of the endometrium.
As estrogen levels rise, a negative
feedback message is sent to the pituitary
to turn off FSH secretions.
Estrogen also causes a positive
feedback mechanism on the secretion of
LH; LH is released when estrogen levels
are high.
Ovulation occurs at
the end of the follicular
phase.
Luteal Phase:
LH causes the corpus luteum to secrete
estrogen and progesterone.
Estrogen and progesterone further the
development of the endometrial lining.
As progesterone and estrogen build up,
another negative feedback mechanism is
activated which inhibits the release of
FSH, LH and GnRH.
The corpus luteum will disintegrate,
estrogen and progesterone levels will
drop, and menstruation will occur.