Communication in Health Care - SBAR Tool
advertisement
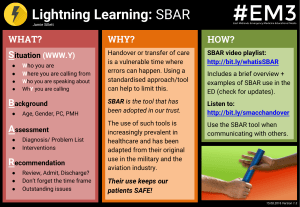
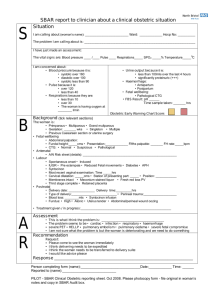
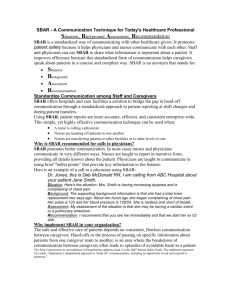
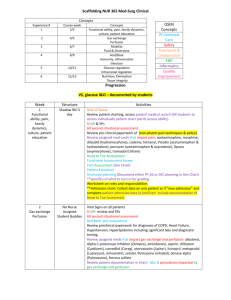
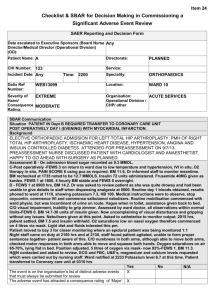
COMMUNICATION IN HEALTH CARE SBAR Tool Learning Objectives 1. To identify the nature and causes of communication breakdown in health care. 2. To understand the SBAR tool and its effectiveness in preventing communication breakdown and promoting patient safety. 3. To develop skill in using SBAR. 4. To identify strategies for implementing SBAR. 5. To understand how SBAR should be used. Patient Safety Primary Purpose Improved communication among health care providers and patient/caregivers will improve the quality and safety of the care the patient receives. National Patient Safety Goal focused on improving the effectiveness of communication among caregivers. The Joint Commission Sentinel event stats found that communication issues were the root cause of about 65% of the sentinel events reported between 19952004. Many of these events resulted in patient death. Enablers/Barriers • Team Work to include, • Resources to include, trust and respect, staffing, equipment communication, and supplies, leadership, environment. inclusiveness. • Responsibility to • Culture to include, include, Organizational leadership, hierarchical (e.g. structures and structures, systems, managing communications and change, corporate and systems approach individual program, staff safety, individual. Communication Errors Contributing Factors Human Performance Limitations Interpersonal Dynamics Hierarchical structures Cultural Differences Gender Differences Disciplinary Differences Individual differences and Filters Team Functioning and the Clinical Environment situational awareness learning environment communication processes/structures Team Functioning and the clinical environment • Situational Awareness • Ineffective • Multiple information Communication Structures • Hand-offs and transitions • Team rounds • Limited Time • Ineffective response to errors sources with multiple players • Incomplete information • Rapid changes with clinical scenarios Consider the impact of: limited memory capacity stress fatigue multi-tasking Consider also: 1. “pecking order” may prevent sharing 2. individuals not confident in own observations and recommendations 3. What does it mean to “question” 4. Culture & Gender influence communication content and style Communication between Disciplines Additional Dynamics between providers to consider: 1. Medicine/Nursing Brief details vs. narrative or descriptive 2. OT-PT Order vs. Flexibility, Judgers vs. perceivers 3. Pharmacy focuses on observable data We bring different filters to work. It is important to identify these differences and develop a shared structure to support effective communication Communication errors are a team and system approach SBAR APPROACH We need to create a culture that examines errors in light of interpersonal dynamics and communication structures WHAT IS SBAR? The SBAR model will be used to facilitate accurate and thorough patient handoff communication between care providers. This will include a focused process in communication with Physicians in relation to clinical situations. SBAR Always identify yourself and the patient at the beginning of an SBAR S=Situation… the problem or concern B=Background the relevant clinical data A=Assessment relay your findings R=Recommendations action or request needed Human Factor response concepts Appropriate Assertion Critical Language Situational Awareness: What are the red flags Create the learning environment including debriefing A COMMON DEBRIEF MODEL IS SBAR Assertion: individuals speak up, and state their information with appropriate persistence until there is clear resolution Assertion Barriers: Power Differences Lack of common mental model Don’t want to look stupid Not sure when you are right Others?? Overcoming Barriers: Get the person’s attention Express Concern State the Problem Propose an Action Reach Decision Critical Language We have a serious problem, stop and listen to me C=I’m Concerned U=I’m Uncomfortable S=This is Unsafe Situational Awareness Maintain the Big Picture Quality of Care Safety Think ahead and plan Discuss contingencies Tune into Red Flags RED FLAGS • Ambiguity • Doesn’t feel right • Poor communication • Boredom • Confusion • Task saturation • Doing something new • Being rushed under pressure • Verbal Violence • Deviating from established norms Create a learning environment: DEBRIEFING After the event/situation ask: What did the team do well? What were the challenges? What will we do differently next time? SBAR EXAMPLES Case SCENARIOS SEE HANDOUTS Successful SBAR Implementation Support from Leadership Teamwork Training Use of Standardized/structured tools Errors are not considered clinical incompetence Team members respond to requests in positive collaborative manner When to use SBAR Time sensitive or critical situations Treatment decisions requiring “same page” collaboration Phone call to MD’s/team members Hand-offs/transitions in care When you need clarity Reminders: Think out loud/sounding board Close the Loop with an action and accountability Be prepared with needed info before making a phone call Expect a response to your request for help USE critical language Support each other using SBAR NEXT STEPS 1. Take this information back to your facility 2. Share this information with the clinical staff 3. Determine the best way to implement SBAR in your facility 4. Share feedback at the April 8th Focus Group meeting 5. Be prepared to fully implement SBAR with your staff by the 28th of April 6. Call for assistance if additional information or education is needed for your facility. QUESTIONS?? CONTACT Michelle Nelson Robin Moreno If additional information or assistance with education is needed. THANK YOU