IPOC - Puget Sound Nursing Informatics (PSNI)
advertisement
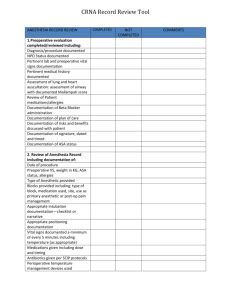
Holly Bowles RN, BSN, Clinical Informatics Specialist Opened in 1960 281 Bed Community Hospital in North Seattle with Level 4 ED/Trauma, Level 2 Neonatal Nursery 1900 Employees, 725 Medical Staff ◦ 34,000 ED Visits ◦ 1300 Births ◦ 11,300 Admissions ◦ 450,547 Outpatient Visits 2013 Statistics Streamline work and be helpful in patient care Reduce redundancies in documentation Ease of use and maintenance of the POC Care coordination: Interdisciplinary Studies have shown that an interdisciplinary approach to care can assist in reducing readmissions, mortality, costs and length of stay while simultaneously increasing communication, collaboration and satisfaction of care providers and patients (Preen et al., 2005) (Vazirani, Hays, Shapiro, & Cowan, 2005). Tool to manage complex patients across multiple admissions Must be evidence-based Previous process was done on paper Diagnosis-based Little interdisciplinary involvement. Plan of Care on the chart was primarily nursing Protocol based system with pre-printed content. Had the ability to add additional information/variances if needed. Interdisciplinary group of clinicians: ◦ Included representatives from Nursing , RT, PT, OT, Speech, Care Management, Food & Nutrition and Pharmacy. Nursing’s members included Clinical Nurse Specialists, Clinical Coordinators, Staff Nurses and Managers. Many meetings and serious work, 2009-2013 Hiatus for CPOE Implementation Early Meetings (2009) ◦ Encouragement to think outside of the box ◦ Hospital was diagnosis-based ◦ Evaluated top ICD-9 codes and DRGs and concluded that it was too large of a number of IPOCs that would be needed ◦ Reviewed NIC/NOC content Used Specialty break downs to help focus the needs ◦ Reviewed Zynx Plans ◦ Decision to proceed with problem-based IPOCs Meetings (2013) ◦ ◦ ◦ ◦ Started in December 2012 Reviewed improved Zynx Plans of Care Reviewed design decisions made in 2009 Reviewed list of requested Plans of Care from 2009 Narrowed list down from 135 to 77 ◦ Held 3 all day design sessions over 1 month along with “homework” for designated staff Hospital wide IPOCs done with entire group Specialty based IPOCs done individually/small groups Interdisciplinary- Therapies, Respiratory Care, Food & Nutrition, Pharmacy, Care Management, Nursing Problem-based pans Easy access to review, initiate and update Evidence based standards using Zynx Standardized Language: SnoMed CT Protocols are incorporated Clinical Notes are associated with Expected Outcomes Unique Clinical Summary Layout to facilitate both staff and provider usage Easier to focus attention on the highest priorities for the patient during this encounter Sample IPOC Clinical Summary Layout Taking us where no Northwest Hospital Staff has gone before….. Can you tell if this patient is progressing toward Expected Outcomes? We see some of what the staff did during this shift, but not where the patient is related to their goals…. Documented in Shift Assessment Documented in MAK Documented in VS/I&O What does this mean??? Progress toward or away from Expected Outcomes Unusual event note- Security issues, family issues, lost belongings Emergent Codes ADT notes Chart by exception Don’t duplicate charting already done Ask: Should this be captured as a problem? Writing a good Clinical Note is a skill which takes thought and practice but it will save time in the long run and our communications will be much improved ! One Giant Step… If NWH policy states that we are a “Documentation by exception system”, Then, we don’t have to do “what we have always done,” So, let’s take back the clock! It is time to leverage the power of technology to improve the quality of care we are providing for our patients! Workflow Engine listens for clinical assessment documentation, lab test results and signed orders, then suggests patient problems based on clinical data entered in Soarian. The workflow listens for the initial plan of care save, then sends an alert to the nurse four hours after patient admission, with a reminder to complete the Plan of Care, if not already done. The workflow monitors for completion of daily Plan of Care Review documentation, and sends a reminder to complete the Plan of Care Review, if not already documented. After patients are discharged the workflow resolves all active Plan of Care problems. Training Sessions: 4 hrs. for RNs, 1.5 hrs. for Therapies Training included “hearts & minds” intro, Plan of Care: create/manage, Clinical Notes, Practice. IPOC Tip Sheet developed at the end of 1st week of post-LIVE support Training Objectives: Navigate established Plans of Care Manage suggested problems Demonstrate how to develop a Plan of Care, select and add interventions and chart to outcomes Use predefined evidence-based Plans of Care to individualize patient care Document a clinical note View Standards (original Plan of Care template) View Plan of Care elements and Clinical Notes in Clinical Summary Note: although they work together, Problems, Expected Outcomes and Interventions are managed separately. Advertising began with the Clinical Support Team talking with staff during rounds Flyers posted throughout the units “Treats” with labels speaking of Plan of Care distributed to all clinical staff Staff Meetings Weekly Announcements Staff embraced the IPOCs/Clinical Notes on the first day. The staged roll out planned for 4 days was done in 2! Couldn’t stop them! Staff became more aware of what they were documenting and questioned processes to stream line their documentation Staff have commented on time saved, ease of use and how it has brought meaning to the plan of care Providers became aware of the IPOCs and asked great questions Questions?