Assessing Professionalism
advertisement
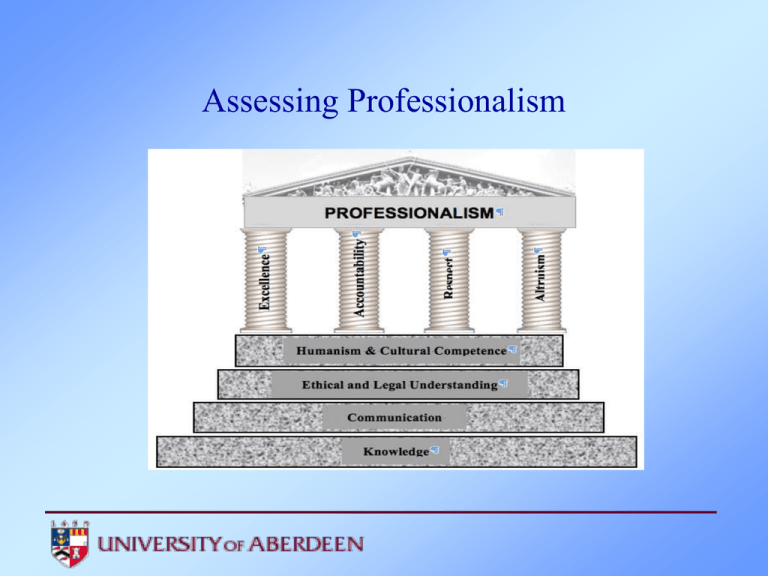
Assessing Professionalism Professional Standards GMC • Duties of a Doctor. • Good Medical Practice (2006, new edition 2012). •Tomorrow’s Doctors (2009) ‘Medical professionalism signifies a set of values, behaviours, and relationships that underpins the trust the public has in doctors’ RCP, Doctors in Society, 2005 Why assess professionalism? • Disciplinary action from medical board was strongly associated with prior unprofessional behaviour in medical school •The types of unprofessional behaviour most strongly linked with disciplinary behaviour were severe irresponsibility and severely diminished capacity for self improvement Papdakis et al 2004&2005 •Requirement for students to demonstrate the development of professionalism in courses regulated by the GMC Why assess professionalism? • Most complaints against doctors are because of conduct not competence • Present behaviour can predict future actions • Students do not arrive at medical school with a full complement of professional behaviours –needing only teaching of medical knowledge and skills • Professionalism does not osmose • All doctors are vulnerable to lapses in professional behaviour and can benefit from explicit systematic attention in this domain • Evidence that there may be a deterioration in professional attitudes from idealism to cynicism Measuring Professionalism Arnold 2002 Academic medicine. • Array of assessment tools, but their measurement properties need to be strengthened • Future research aimed at exploring rigorous qualitative techniques, refine quantitative techniques eg OSCE and evaluate separate elements of professionalism • Should measurement tools be tailored to the stage of medical career and examine how the environment can support or sabotage the assessment of professional behaviour are central issues Measuring professionalism Ottawa conference 2010 recommendations • Individual characteristics; looking at attributes, capacities and behaviours eg psychometric tests, observable behaviour tests such as PAT (peer assessment tool), critical incident reports, MSF(multi source feedback). 88 tools in the literature • Interpersonal process;interactions with other individuals and within different contexts, collective professional values • Macro – social level; social responsibility and morality Interactions of these levels as a continuum, feedback required, and needs diversity of approach. Group work • What system do you have for assessing professionalism? • What tools do you use to assess your outcomes? Aberdeen Experience • Student Ethical Code • Year 1PPD. Series of 4 lectures, 2 tutorials and 1 seminar. Submit a single activity each term for their PPD portfolio, assessed formatively by a tutor and possibly the course coordinator and external examiner. Class certificate not issued if they fail to submit by stated deadline, absent from 10% or 2 sessions or more without good cause. All portfolio activities to be submitted to ‘Turnitin’ before uploading for tutor Aberdeen Experience •Year 2 PPD. Series of 2 seminars and 1 lecture. Submit a single activity each term for their portfolio. Same conditions apply as in Year 1. •Year 3 PPD One seminar on ‘Professionalism:challenges for students’ One lecture on ‘Careers’ Submit a single activity each term for their portfolio Same conditions apply as in Year 1. Aberdeen Experience GP Block Year 4 and 5 Maintaining Trust Evidence of maturity, professionalism and probity in general behaviour and actions Consider attendance, honesty, dress and manners. Refer to Dress Code found in Handbook Always seen as acting appropriately with regards punctuality, honesty, dress and general professional behaviour towards patients and staff Outstanding Present as honest amd have good general professional behaviour towards patients and staff but not exemplary eg with regards punctuality, dress and manner Good Dishonesty or rude/inappropriate manner towards patients and/or staff. Unacceptable professional manner. Fail Aberdeen Experience Professional Practice Block Year 5 •Four week programme, split with two weeks start of year and two weeks end of year •May be assessed in final OSCEs •Students are expected to attend all sessions, failure may result in withdrawal of class certificate •10 key themes. Patient safety;non technical skills. Handover and communicating with colleagues.Written communication.Prescribing skills. How to manage stress. Medical careers:foundation applications.Domestic abuse. End of life. Radiation protection. Clincal ethic and law. Group work • Reviewing the tools for assessing professionalism Remediation Attitudes v Behaviours • • • • Is it possible? Relationship between attitude and behaviour is complex Behaviour is influenced by attitude Measures of general attitude do not necessarily predict specific behaviours BUT • They do have a good correlation to behaviour over a period of time in a range of situations and contexts ( called aggregation principle) Conclusion • Changing behaviour probably means changing underlying fundamental beliefs • Understanding ways of changing professional attitude behaviour is for the future Thanks Dr Kathy Boursicot and Dr Trudie Roberts. St George’s Advanced Assessment Course General Medical Council (2006) Good Medical Practice GMC:London Royal College of Physicians(2005) Doctors in Society:medical professionalism in a changing world RCP: London Johnston J, Cupples M, Mcglade K,and Steele K(20110 Medical students’attitudes to professionalism:an opportunity for the GP tutor?. Education in Primary Care 22:321-7