File
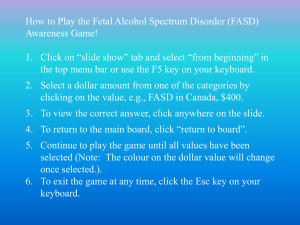
advertisement

“BEHAVIOURS” IN THE CLASSROOM BRIDGING THE GAP BETWEEN TEACHER AND PAEDIATRICIAN Dr. Aven Poynter Financial Disclosures None with respect to mental health OBJECTIVES 1. Recognize symptoms that warrant referral/investigation 2. Learn what you can do to assist in diagnosis 3. Review suggestions from medical and mental health professionals to support the child in the classroom Diagnosis vs Label Naming a Condition • Helps understand the feelings & behaviours • Helps find treatment and support Labeling a Person • You are an “ADHD” person • You will carry this label forever 2 Traditional Approaches to Mental Health Problems in School • • Fix the school Fix the kid Dr. S. Kutcher PARENT TEACHER CHILD COMMUNITY RECOURCES DOCTOR Do You Have a Pupil Who? • • • • • • Easily distracted Developmental dysmaturity Feels different Doesn’t consider consequences Doesn’t listen Doesn’t follow through Do You Have a Pupil Who? • • • • • • Difficulty organizing Difficulty with transitions Poor impulse control Acts hyperactive Sleep disturbance Indiscriminately affectionate Do You Have a Pupil Who? • • • • • • Lack of eye contact Lies about the obvious Won’t/can’t learn Abnormal speech/incessant chatter Wide mood swings Problems with social interactions Do You Have a Pupil Who? • • • • • • Over/under responsive to stimuli Perseverates, inflexible Escalates in response to stress Poor problem solving Difficulty seeing cause and effect Difficulty initiating/following through Do You Have a Pupil Who? • Manages time poorly, lack of comprehension of time • Speech/language processing difficulties • Loses temper • Argues with adults, actively defies • Blames others, resentful 15% of children and adolescents have a mental health (psychiatric) disorder Age at Diagnosis 14 12 10 8 6 4 2 0 Autism ADHD Anxiety Depression ADHD Attention Deficit Hyperactivity Disorder ADHD • • • • 5 – 10% of children Boys > Girls Described 200 years ago! A Neurobiological disorder NOT A Behavioural disorder ADHD Impairments in • Executive function • Working memory • Processing speed ADHD • Combined Type • Inattentive Type • Hyperactive-Impulsive Type ADHD Inattentiveness • • • • • • • • • • Easily distracted Difficulty concentrating for reasonable length of time Fails to pay close attention to details, makes careless mistakes Loses belongings Difficulty organizing activities Does not seem to be listening Problems following instructions Difficulty completing activities Difficulty getting started, especially if a challenging activity Often forgetful- forgets to write things down, forgets routines ADHD Hyperactivity-Impulsivity • • • • • Often squirmy, fidgety Constantly moving and on the go Makes a lot of noise Interrupts Blurts out answers to questions before hearing the whole question • Talks when supposed to be quiet • Runs about and climbs when not appropriate • Can’t wait in line, can’t await turn ADHD • Started before age 7 years • Duration more than 6 months • Difficulties in more than one place, like both at school and at home • Significantly impair the child • Are not related to another disorder • Video – brain chemistry ADHD POSITIVES • • • • • • • Spontaneous Creative Social butterfly Can multitask Can think outside the box Enthusiastic Daring ODD Oppositional Defiant Disorder ODD • Learned behaviour • Interaction between child, parent, environment ODD • • • • • Loses temper Argues with adults Defies/refuses adult requests Defies rules Deliberately annoys others ODD • Blames others for his mistakes or misbehaviour • Touchy or easily annoyed • Angry and resentful • Spiteful or vindictive DCD Developmental Co-ordination Disorder DCD • 5% of children • Boys > Girls • DCD is a prevalent yet underrecognized movement skill disorder that significantly affects everyday functioning DCD • Coordination difficulties affect child's ability to perform everyday tasks • A discrepancy is found between intellectual capabilities and motor abilities • DCD persists into adolescence and adulthood DCD • DCD is commonly seen with other developmental conditions including ADHD, LD, speech/language disorders, and behavioural disorders • DCD may contribute to secondary emotional, social and mental health problems DCD Has troubles with daily activities • Putting on and taking off clothing • Tying shoelaces • Managing zippers, buttons and snaps • Using eating utensils • Cutting with scissors • Catching a ball DCD • • • • moves awkwardly seems clumsy or poorly coordinated frequently trips, or drops things prints or writes poorly, and with much effort DCD • avoids participation in physical or motor-based activities • has difficulty learning and transferring new motor skills DCD • The motor-based activities of school are challenging for children with DCD • Teachers are in a unique position to identify children with motor problems • Boys tend to be identified more often than girls, perhaps related to behavioural issues • DCD remains an under-recognized disorder DCD Activity • Ball skills • Fine motor skills with workgloves on LD Learning Disabilities Learning Disabilities • • • • “Learning Difference” 10% of population 15% of Canadians illiterate 42% of Canadians illiterate or semi-literate Learning Differences • Dys – lexia – Processing Language • Affects reading, writing, spelling Learning Differences • Dys – calculia – Math skills • Computation • Remembering math facts • Concepts of time and money Learning differences • Dys – graphia – Written expression • Messy handwriting • Poor spelling • Can’t get thoughts onto paper Learning Differences • Auditory Processing Disorders • Visual Processing Disorders Learning Disabilities • Discrepancy between intellect and achievement • Can often result in emotional, behavioural and attentional problems CAPD Central Auditory Processing Disorder CAPD • Normal hearing • Can’t filter out irrelevant noise • Difficulty understanding what s/he is hearing • Doesn’t seem to pay attention in the classroom ODD ADHD DCD LD How can you help sort these out? • • • • • • Discuss concerns with student’s parent Describe concerns and observations Don’t mention a diagnosis Recommend vision exam Recommend hearing test Recommend general medical exam How can you help to sort these out? • Review school file • Consider consulting – – – – – Counsellor Learning Assistance (Resource) Teacher Speech & Language Therapist Behaviour Resource Teacher School Psychologist Useful Information for me • • • • • • Reports of above assessments Brief narrative of your observations All previous report cards for student SNAP rating scale Conners’ rating scale Weiss rating scale What I will ask of You • • • • • **Psychoeducational Assessment** Occupational Therapy Assessment Speech & Language Assessment IEP Resource room block FASD Fetal Alcohol Spectrum Disorder ARND Alcohol-Related Neurodevelopmental Disorder FASD • First described 1968 • Prenatal alcohol exposure • Constellation of physical and neurodevelopmental abnormalities • Diagnosis by multi-disciplinary team • 1:100 but under-diagnosed FASD • A permanent brain injury • We see the intellectual effects and the BEHAVIOURAL effects • http://www.fasdoutreach.ca/ FASD • People with FASD can “talk the talk but not walk the walk” • We need to recognize that it is not that the child with FASD won’t do it, but can’t do it FASD Primary Disabilities • Lower developmental age • Speech and language problems • Fine and gross motor difficulties • Slow processing • Memory problems -> confabulation and ownership FASD Primary Disabilities • Impulsivity • Distractibility • Poor abstract thinking – Generalization – Time, money, space • Cause and effect FASD Secondary disabilities • Mental health • School problems -> drop out • Inappropriate sexual behaviour • Trouble with law • Employment FASD Secondary Disabilities • Substance abuse • Housing • More apparent with age FASD Many people with FASD have strengths which mask their cognitive challenges. • • • • • • • • Highly verbal Bright in some areas Artistic, musical, mechanical, athletic Friendly, outgoing, affectionate Determined, persistent Helpful Generous Good with younger children ASD Autism Spectrum Disorder ASD Pervasive Developmental Disorders • Autism Spectrum Disorder • Asperger’s Disorder • PDD Not Otherwise Specified Prevalence changing – 1:150 to 1:100 ASD • Leo Kanner – Autism – 1943 • Hans Asperger –Asperger’s – 1944 • “Disorders of Empathy” ASD 1. Disturbance in social interaction 2. Impairments in communication 3. Restricted, repetitive and stereotyped patterns of behaviour, interests, and imaginative activities AUTISM Qualitative impairment in social interaction • No use of noverbal behaviours such as eye contact, facial expressions, gestures • Failure to develop peer relationships • Does not share enjoyment/interests, • Lack of social/emotional reciprocity AUTISM Impairment in Communication • Lack of spoken language, not compensated by gesturing • If has speech, inability to initiate or sustain conversation • Stereotyped, repetitive, or idiosyncratic language • Lack of spontaneous make-believe play AUTISM Restricted, repetitive, stereotyped behaviour and interests • Encompassing preoccupation • Inflexible adherence to nonfunctional routines or rituals • Repetitive motor mannerisms • Preoccupation with parts of objects AUTISM • Usually also mental retardation • Sometimes special talents • Cannot understand that other people think and feel • Results in extreme deficits in empathy • Sensory regulation disorders ASPERGER’S DISORDER • Qualitative impairment in social interaction • Restricted, repetitive, stereotyped patterns of behaviour, interests and activities • Normal intellect • No delay in early language acquisition Asperger’s Disorder • Seem highly intelligent • Like a “little professor” • Detailed knowledge about specific topic of interest • Relate better to adults • Want friends, can’t make/be friends Asperger’s disorder • • • • • • Concrete Unusual use of language Difficulty understanding metaphors Difficulty understanding jokes Difficulty reading facial expressions Develop Anxiety Tourette’s Syndrome Tourette’s Syndrome • 1825 – described by Dr. Itard • 1883 – described by Dr. George Gilles de la Tourette Tourette’s Syndrome • Chronic motor and vocal tics – Onset usually age 6 – 8 years – Simple tics and complex tics – Coprolalia is rare Tourette’s Syndrome • Often also have – Obsessive-Compulsive Disorder – ADHD RDSP Regulation Disorder of Sensory Processing RDSP • Difficulties in areas of – Sensory response – Motor responses – Behavioural responses • Often see difficulties in – sleep, eating, elimination – Language – Cognitive function RDSP • Hypersensitive subtype – Over-reactive to touch, sound, smell, taste, visual stimuli – Fearful & cautious or negative/defiant – May reject movement -> difficulty with motor planning and play RDSP • Hyposensitive/Under-responsive Subtype – Under-reactive to sound, taste, smell, touch, proprioception, visual stimuli – Withdrawn – Seek repetitive sensory patterns – Decreased imaginative play RDSP • Sensory Stimulation seeking/impulsive subtype – – – – Impulsive Disorganized behaviour Poor motor planning -> accident prone Looks like ADHD, but earlier onset Anxiety Disorders Anxiety Disorders • • • • Separation Anxiety Disorder Obsessive Compulsive Disorder Post-Traumatic Stress Disorder Panic Disorder Anxiety Disorders • • • • • • School avoidance Tummy-aches & headaches Inattentiveness Hyperactive behaviour Defiance Crying Anxiety • May be primary • Often co-exists with – – – – – – ADHD DCD LD’S FASD ASD RDSP Anxiety Prevention • FRIENDS program Screening if you suspect • SCARED In the Classroom Classroom Environment • Same for everyone – – – – – Uncluttered Not too noisy Post schedule Organize supplies Study carrell • Seat distractible students near you Classroom Strategies • Allow movement – – – – – Errands wiggle cushion Squeeze ball Arrange a cue with hyperactive child Allow wandering Classroom Strategies • • • • Quiet class before giving instructions Visual and verbal together Establish eye contact One instruction at a time, allow time to process before next instruction Classroom Strategies • Create predictable schedules and routines for: – – – – transitions turning in homework asking for help getting supplies or materials Classroom Strategies • Break assignments into small chunks • Reduce number of questions – sufficient to demonstrate knowledge • Close support with agenda book and organizing homework • Provide pre-printed notes Classroom Strategies • • • • • • • Clear rules Consider token system Lots of short-term, achievable goals Immediate feedback Positive feedback for good behaviour Positive feedback for successes Warn ahead for transitions Classroom Strategies • Technology – FM system – Computer - keyboarding - spellcheck - voice software Audiotapes • Old-fashioned scribe Classroom Strategies • Consult OT when sensory issues involved as therapy needs to be individualized • ABA is not for everyone with autism Classroom Strategies • PE – same team position for child with problems with motor skills • Capitalize on individual talents eg music/dance Modify the task Alter your expectations Teaching strategies Change the environment Help by understanding